Antibody-Mediated Rejection Can Be Assessed by Histology When DSA Is Unknown or Negative.
1Laboratory Medicine and Pathology, University of Alberta, Edmonton, AB, Canada
2Department of Medicine, University of Alberta, Edmonton, AB, Canada.
Meeting: 2016 American Transplant Congress
Abstract number: C21
Keywords: Gene expression, Kidney transplantation, Rejection
Session Information
Session Name: Poster Session C: Antibody Mediated Rejection: Session #1
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Diagnosis of antibody-mediated rejection (ABMR) in kidney transplants currently requires the presence of donor-specific antibody (DSA) and histologic lesions above somewhat arbitrary cutoffs. DSA is sometimes negative in otherwise ABMR-like biopsies, or is not available. Dichotomous lesion-based rules may also lose relevant information regarding the true disease state. To address these problems, we assessed the likelihood of ABMR using logistic regression. This depends less on rules and more on the overall relationship between the key variables (lesions, DSA, time post-transplant). We analyzed a set of 703 prospectively collected indication biopsies.
Probability of ABMR can be estimated either by an equation or its graphical equivalent, the nomogram. Figure 1 shows a nomogram for predicting molecular ABMR (samples called ABMR+ through microarray analysis) using the histoclinical variables that survived backward elimination. 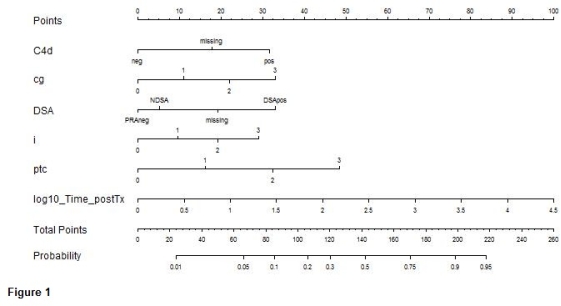
These predictors are shown on the left of the graph. For each value of a variable, a score is read from the "Points" line, and the sum of these scores across all variables is looked up on the "Total Points" line. Finally, the corresponding probability of ABMR is read off the "Probability" line.
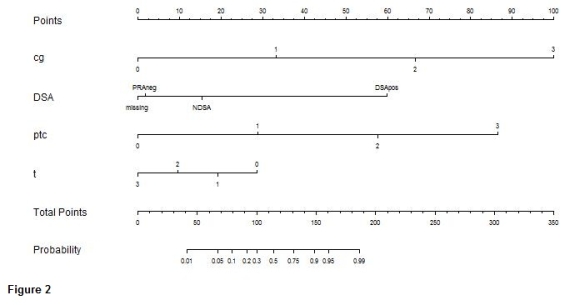 Figure 2 shows a nomogram for predicting biopsies diagnosed histologically (rather than molecularly) as having ABMR.
Figure 2 shows a nomogram for predicting biopsies diagnosed histologically (rather than molecularly) as having ABMR.
Both versions found that many DSA negative biopsies had high ABMR probabilities, as did some that didn't meet all the lesion requirements. The reverse was also true – some ABMR diagnoses had low ABMR probabilities.
We conclude that a data-driven approach to ABMR diagnosis allows a probabilistic assessment which does not rely on strict adherence to the current set of rules. These results also argue that the current requirement that ABMR must have detectable DSA is not correct.
CITATION INFORMATION: Reeve J, Halloran P. Antibody-Mediated Rejection Can Be Assessed by Histology When DSA Is Unknown or Negative. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Reeve J, Halloran P. Antibody-Mediated Rejection Can Be Assessed by Histology When DSA Is Unknown or Negative. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/antibody-mediated-rejection-can-be-assessed-by-histology-when-dsa-is-unknown-or-negative/. Accessed June 30, 2025.« Back to 2016 American Transplant Congress
