Activation of Th17 and Chronic Renal Allograft Rejection in Nonhuman Primates
Transplant Center, Massachusetts General Hospital, Boston, MA.
Meeting: 2015 American Transplant Congress
Abstract number: D7
Keywords: Kidney transplantation, Primates, Rejection, T cell activation
Session Information
Session Name: Poster Session D: Costimulation and Signaling in Lymphocytes
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Background: We have previously reported successful induction of renal allograft tolerance in nonhuman primates (NHP) via a mixed chimerism approach. Although donor specific Th1 and Th2 unresponsiveness were observed in these NHP recipients, approximately 30% of recipients eventually developed chronic rejection (CR). Therefore, an alternative pathway is considered to be operative in the development of CR. In this study, we investigated the role of Th17 cells in the pathogenesis of chronic renal allograft rejection
Methods: Cynomolgus monkeys underwent combined kidney and bone marrow transplantation after treatment with a nonmyeloablative conditioning regimen. No immunosuppression was given after one month. Renal allograft biopsies from recipients with tolerance (TOL: n=10), chronic rejection (CR: n=14), and acute cellular rejection (ACR: n=6) were studied for mRNA expression of various cytokines and transcription factors. Biopsies from recipients with stable renal allograft function under conventional immunosuppression (IS: n=7) were also studied. Immunohistochemical staining with Foxp3, RORγt and IL-17 was also examined.
Results: Messenger RNA levels of RORγt and IL-6 were significantly higher in CR than those in TOL(p=0.006 and 0.024, respectively)), while TGF-β and TNF-α were higher in TOL than in CR (p=0.01 and 0.001). It should be noted that there is no single renal allograft with detectable RORγt in the TOL group. Although statistically not significant, IL-17 levels tend to be higher in CR (Fig.1). Immunohistochemical staining of these renal allografts also showed positive IL-17 staining in the glomerulus of the renal allograft with CR (Fig. 2 left panel, arrows), but not in the tolerant renal allografts (Fig. 2 right panel).
Conclusion: These results suggest that a RORγt dependent process, potentially the Th17 pathway, may be important in the pathogenesis of chronic renal allograft rejection. 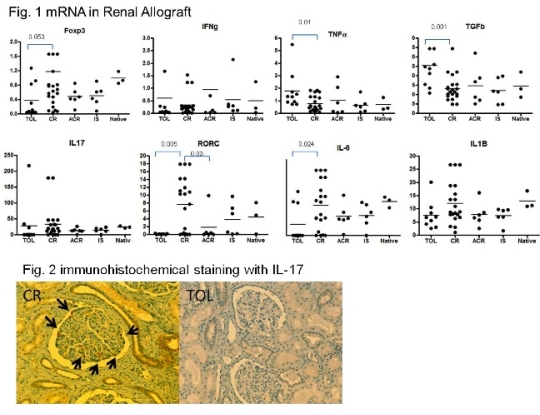
To cite this abstract in AMA style:
Hotta K, Aoyama A, Putheti P, Yamada Y, Ohura T, Colvin R, Cosimi B, Benichou G, Strom T, Kawai T. Activation of Th17 and Chronic Renal Allograft Rejection in Nonhuman Primates [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/activation-of-th17-and-chronic-renal-allograft-rejection-in-nonhuman-primates/. Accessed March 1, 2026.« Back to 2015 American Transplant Congress
