A Novel Mismatch That Modulates the Innate Alloresponse Risk Stratifies Renal Transplant Patients
Thomas E. Starzl Transplantation Institute, UPMC, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 1584
Keywords: Graft failure, Kidney transplantation, Outcome
Topic: Basic Science » Basic Clinical Science » 17 - Biomarkers: Clinical Outcomes
Session Information
Session Name: Biomarkers: Clinical Outcomes
Session Type: Poster Abstract
Date: Tuesday, June 7, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Donor polymorphism in the gene encoding signal regulatory protein alpha (SIRPα) is a key modulator of the recipient’s innate alloresponse. Here, we investigated the impact of SIRPα polymorphism and the resultant SIRPα donor-recipient (D/R) mismatch (m/m) on early and late graft outcomes after renal transplantation.
*Methods: 188 D/R pairs (136 LD & 52 DD) transplanted between 2013 and 2018 were genotyped. SIRPα mismatch was assessed and correlated with early and late transplant outcomes. Patients underwent protocol biopsies (3mos and 12mos) and DSA was screened at 0,1,3,6 and 12mos.
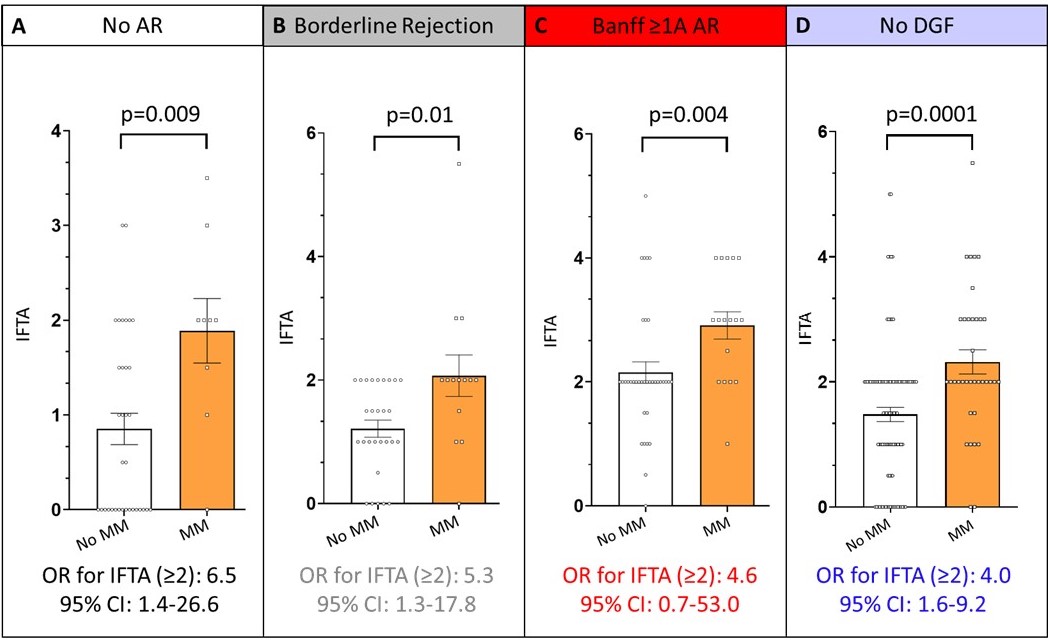
*Results: Analysis of SIRPα variants A and B, the two most common variants with different CD47 binding affinities showed that D/R SIRPα mismatch was present in 29% of patients. Mismatches were subclassified as A (seen in 12%) or B (seen in 17%) when these particular variants were present in the donor but not the recipient. Baseline clinical characteristics were comparable between those with or without SIRPα mismatch. SIRPα m/m was associated with more DGF (OR 4.0, 95% CI 1.5-10.3). Although there was no association between SIRPα m/m and either DSA or acute rejection (AR), patients with B m/m had a statistically non-significant trend towards greater incidence of borderline and Banff ≥1A AR (matched: Borderline AR: 28%; Banff ≥1A AR: 35% vs. B m/m: Borderline AR: 38%; Banff ≥1A AR: 46%). SIRPα m/m however was associated with significantly greater cumulative IFTA scores at 1year (mean IFTA score matched 1.5 vs. m/m 2.4, p<0.0001), and a greater proportion of m/m patients had moderate to severe IFTA (matched 10% vs. m/m 38%, p=0.0001). Importantly, both A and B m/m were associated with a greater incidence of moderate to severe IFTA compared to matched patients (matched 10% vs. A m/m 37% vs. B m/m 42%, p=0.0007). As shown in Figure 1, the association between SIRPα m/m and worse IFTA was independent of the grade of acute rejection or DGF. This independent association was further confirmed in a multivariable Cox regression model (OR: 5.0, 95% CI 2.1-11.9). Finally, SIRPα m/m was associated with worse 7-year death censored graft survival compared to patients without a mismatch (matched: 96% vs. m/m 77%, p=0.04). This association was more pronounced in patients with B m/m (matched 96% vs. A m/m 90% vs. B m/m 73%, p=0.01).
*Conclusions: This exploratory study highlights the utility of SIRPα m/m as a new risk stratification tool to identify patients at risk for premature allograft scarring and poor long-term outcomes.
To cite this abstract in AMA style:
Dai H, Daya KAbou, Oberbarnscheidt M, Mehta R, Macedo C, Metes D, Xu Q, Zeevi A, Randhawa P, Lakkis F, Cherukuri A. A Novel Mismatch That Modulates the Innate Alloresponse Risk Stratifies Renal Transplant Patients [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/a-novel-mismatch-that-modulates-the-innate-alloresponse-risk-stratifies-renal-transplant-patients/. Accessed July 18, 2025.« Back to 2022 American Transplant Congress