A Novel Approach to Preserve Pancreatic Islet Grafts in Extrahepatic Space for Reversal of Diabetes Using Parathyroid Gland Co-Transplantation
UCSF, San Francisco, CA.
Meeting: 2018 American Transplant Congress
Abstract number: 484
Keywords: Engraftment, Graft survival, Insulin, Islets
Session Information
Session Name: Concurrent Session: Pancreas and Islet - 2
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:18pm-3:30pm
Presentation Time: 3:18pm-3:30pm
Location: Room 4C-3
Intro: Islet transplantation can cure type 1 diabetes; however, multiple donors are needed due to extensive perioperative loss of islets away from their native blood supply. In comparison, parathyroid gland (PTG) autotransplantation in the subcutaneous (SQ) and intra-muscular (IM) sites is an established surgical procedure. In this study, we aim to exploit the neoangiogenic and paracrine hormonal factors made by PTG for preservation of mature islet and stem cell grafts.
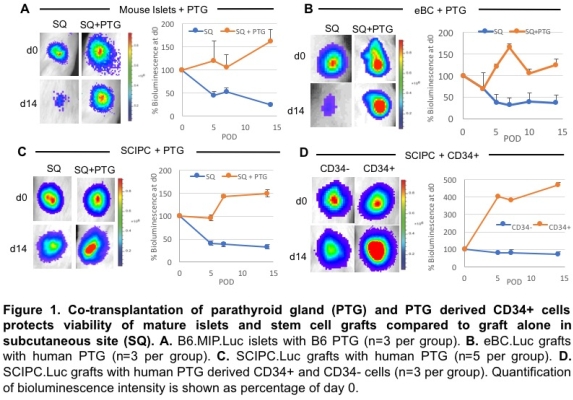
Methods: Luciferase-expressing mouse islets (B6.MIP-Luc), Stem-Cell-derived Insulin-Producing Cell (SCIPC.Luc) and enhanced Beta Cell (eBC.Luc) grafts were co-transplanted with PTG in SQ and IM. PTG derived CD34+ cells were FACS purified. Mice were made diabetic with STZ.
Results: Co-transplantation of PTG with mouse islets, SCIPC's and eBC's in the SQ and IM resulted in preservation of graft mass in comparison to significant graft loss when transplanted alone (Figure 1A-C). PTG-derived CD34+ cells were as effective as whole PTG in preserving graft mass whereas CD34- cells provided minimal benefit (Figure 1D). The islet-preserving effects were associated with marked enhancement of graft vascularization and protection of beta-cell death by PTG-secreted factors.
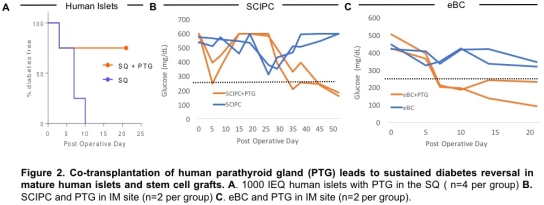
Moreover, PTG co-transplantation led to diabetes reversal using human islets (1000IEQ) in SQ in 1 week, SCIPC in IM in 4 weeks, and eBC in IM in 1 week (Figure 2).
Conclusion: We present a novel co-transplantation of PTG with mature islets and stem-cell derived beta cells leads to significantly increased survival and reversal of diabetes in SQ and IM. Furthermore, the islet-protective activities of PTG resides in CD34+ progenitor cells. The results of this study open many potential future clinical trials in auto, allo, xeno or stem-cell based islet transplants.
CITATION INFORMATION: Ward C., Faleo G., Nair G., Duh Q., Hebrok M., Chang W., Stock P., Tang Q. A Novel Approach to Preserve Pancreatic Islet Grafts in Extrahepatic Space for Reversal of Diabetes Using Parathyroid Gland Co-Transplantation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ward C, Faleo G, Nair G, Duh Q, Hebrok M, Chang W, Stock P, Tang Q. A Novel Approach to Preserve Pancreatic Islet Grafts in Extrahepatic Space for Reversal of Diabetes Using Parathyroid Gland Co-Transplantation [abstract]. https://atcmeetingabstracts.com/abstract/a-novel-approach-to-preserve-pancreatic-islet-grafts-in-extrahepatic-space-for-reversal-of-diabetes-using-parathyroid-gland-co-transplantation/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress