The Differential Effect of HLA-DQ Mismatching on Renal Allograft Survival in Zero HLA-A,B,DR Mismatched Deceased Donor Transplants
1University of Florida, Gainesville
2University of Kansas, Kansas City.
Meeting: 2015 American Transplant Congress
Abstract number: A93
Keywords: Graft survival, HLA matching, Kidney transplantation, Sensitization
Session Information
Session Name: Poster Session A: Kidney Antibody Mediated Rejection
Session Type: Poster Session
Date: Saturday, May 2, 2015
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Exhibit Hall E
The role of HLA-DQ matching in renal graft survival is not well understood and difficult to interpret in the presence of other HLA antigen mismatches. However in recipients of zero HLA-A,B,DR mismatched (0ABDR) transplants, it may be easier to evaluate the effect of HLA-DQ mismatching on graft survival. We hypothesize that in recipients of 0ABDR mismatched deceased donor kidneys, zero DQ mismatches (0DQMM) will provide a greater graft survival benefit than ≥1 DQ mismatches (≥1DQMM).
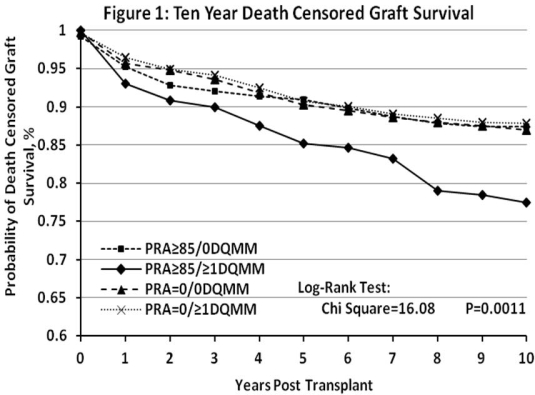
Methods: This is a SRTR database retrospective analysis of adult recipients of a first time solitary 0ABDR deceased donor kidney transplant from 1999-2012. Highly sensitized (PRA≥85) and unsensitized (PRA=0) subjects were stratified by DQ mismatches (0DQMM v. ≥1DQMM). The primary outcome was 10-year death censored graft survival. A multivariate Cox model was used to identify risk factors for graft loss.
Results: In recipients of 0ABDR deceased donor grafts; 519, 234, 1781, and 960 subjects were identified as PRA≥85/0DQMM (group 1), PRA≥85/≥1DQMM (group 2), PRA=0/0DQMM (group 3), and PRA=0/≥1DQMM (group 4) respectively. Kaplan-Meier analysis shows poorer graft survival with ≥1DQMM in subjects with PRA≥85, but not with PRA=0 (Fig. 1). After covariate adjustment, our multivariate Cox model shows that group 2 is associated with a greater risk of graft failure, but no difference is seen with groups 1, 3, and 4 (Table 1).
Conclusion: Our data suggests that DQ mismatching may impact graft survival in highly sensitized patients, but not in unsensitized patients. However, these results might also arise from mismatches at the DP or other nonstandard HLA loci. More complete HLA typing beyond HLA-A,B,DR antigens in highly sensitized recipients of 0ABDR kidneys may be beneficial and may guide future allocation of these grafts.
| Selected Covariates | p value | Hazard Ratio | 95% Confidence Interval | |||
| Lower limit | Upper limit | |||||
| PRA≥85/0DQMM | 0.27 | 1.21 | 0.86 | 1.71 | ||
| PRA≥85/≥1DQMM | 0.01 | 1.62 | 1.10 | 2.38 | ||
| PRA=0/0DQMM | Reference Group | |||||
| PRA=0/≥1DQMM | 0.97 | 1.00 | 0.77 | 1.29 | ||
To cite this abstract in AMA style:
Casey M, Wen X, Rehman S, Santos A, Goldstein S, Andreoni K, Kaplan B, Womer K. The Differential Effect of HLA-DQ Mismatching on Renal Allograft Survival in Zero HLA-A,B,DR Mismatched Deceased Donor Transplants [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/the-differential-effect-of-hla-dq-mismatching-on-renal-allograft-survival-in-zero-hla-abdr-mismatched-deceased-donor-transplants/. Accessed February 20, 2026.« Back to 2015 American Transplant Congress
