Pancreas-Derived Mesenchymal Stem Cells from Chronic Pancreatitis Patients Enhance Islet Graft Function
1Baylor Research Institute, Dallas, TX
2Baylor University, Waco, TX
3Baylor Annette C. and Harold C. Simmons Transplant Institute, Dallas, TX.
Meeting: 2015 American Transplant Congress
Abstract number: 365
Keywords: Graft function, Graft survival, Islets, Stem cells
Session Information
Session Name: Concurrent Session: Islet Transplantation: Basic
Session Type: Concurrent Session
Date: Tuesday, May 5, 2015
Session Time: 2:15pm-3:45pm
 Presentation Time: 2:39pm-2:51pm
Presentation Time: 2:39pm-2:51pm
Location: Room 121-C
PURPOSE: Islet transplantation represents a promising procedure to reverse or prevent diabetes. However, significant mass of islet graft is lost within hours of transplantation due to an acute inflammatory response. Mesenchymal stem cells (MSCs) have been shown to protect islets from inflammation and have capabilities to regenerate islet tissue in animal models. We hypothesized that the inflamed pancreas in chronic pancreatitis (CP) patients is enriched with MSCs that are programmed to mediate inflammatory protection and tissue restoration processes.
METHODS: MSCs from CP patients (n=14) having autologous islet transplantation following total pancreatectomy were isolated from pancreatic remnant tissue recovered during clinical islet isolation procedures. Pancreas-derived MSCs (PMSCs) (∼1X10 6 ) were co-transplanted with isolated human islets (∼1500) into kidney capsules of nude mice with streptozotocin (STZ)-induced diabetes and islet grafts were assessed for function. PMSCs were compared with bone marrow derived MSCs (BMSCs) for capabilities to suppress islet inflammation and differentiate into insulin-producing cells.
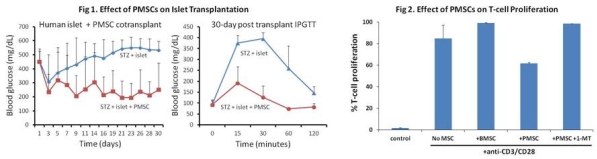
RESULTS: PMSCs co-transplanted with a marginal dose of human islets reversed hyperglycemia and restored IPGTT profiles in diabetic mice (n=5) (Fig 1). PMSCs showed higher potency compared to BMSCs in the induction of genes including PDX-1, NeuroD1, NKx6.1, MafA, GLUT2, and insulin for beta-cell differentiation and conversion into insulin-producing cells. PMSCs also had an enhanced capacity to suppress (27.5 ± 1.2%) T-cell proliferation by a mechanism requiring expression of indoleamine-2-3-dioxygnease (IDO) (Fig 2).
CONCLUSIONS: PMSCs have a high potency to 1) suppress islet inflammation, 2) enhance islet graft function, and 3) differentiate into insulin-producing cells. Their use as adjunctive therapy in clinical islet autologous and allogeneic transplantation should be explored.
To cite this abstract in AMA style:
Lawrence M, Kunnathodi F, Borenstein-Auerbach N, Yoshimatsu G, Kanak M, Shahbazov R, Takita M, Levy M, Naziruddin B. Pancreas-Derived Mesenchymal Stem Cells from Chronic Pancreatitis Patients Enhance Islet Graft Function [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/pancreas-derived-mesenchymal-stem-cells-from-chronic-pancreatitis-patients-enhance-islet-graft-function/. Accessed February 18, 2026.« Back to 2015 American Transplant Congress
