Recipient MCPggaac Haplotype is Associated with Poor Graft Survival in Recipients with De Novo Thrombotic Microangiopathy
1Dept. of Nephrology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic, 2Dept. of Medicine and Hematology, Semmelweis University, Budapest, Hungary, 3Transplant Laboratory, Institute for Clinical and Experimental Medicine, Prague, Czech Republic
Meeting: 2022 American Transplant Congress
Abstract number: 118
Keywords: Gene expression, Gene polymorphism, Graft survival, Kidney transplantation
Topic: Clinical Science » Kidney » 47 - Kidney Complications: Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Chronic Antibody Mediated Rejection & Immune Mediated Late Graft Failure
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:20pm-6:30pm
Presentation Time: 6:20pm-6:30pm
Location: Hynes Room 302
*Purpose: De novo thrombotic microangiopathy (TMA) is associated with poor kidney graft survival. We aimed to assess the role of common complement haplotypes in kidney transplant recipients (KTR) with de novo TMA, their corresponding donors, and KTR of paired kidney grafts.
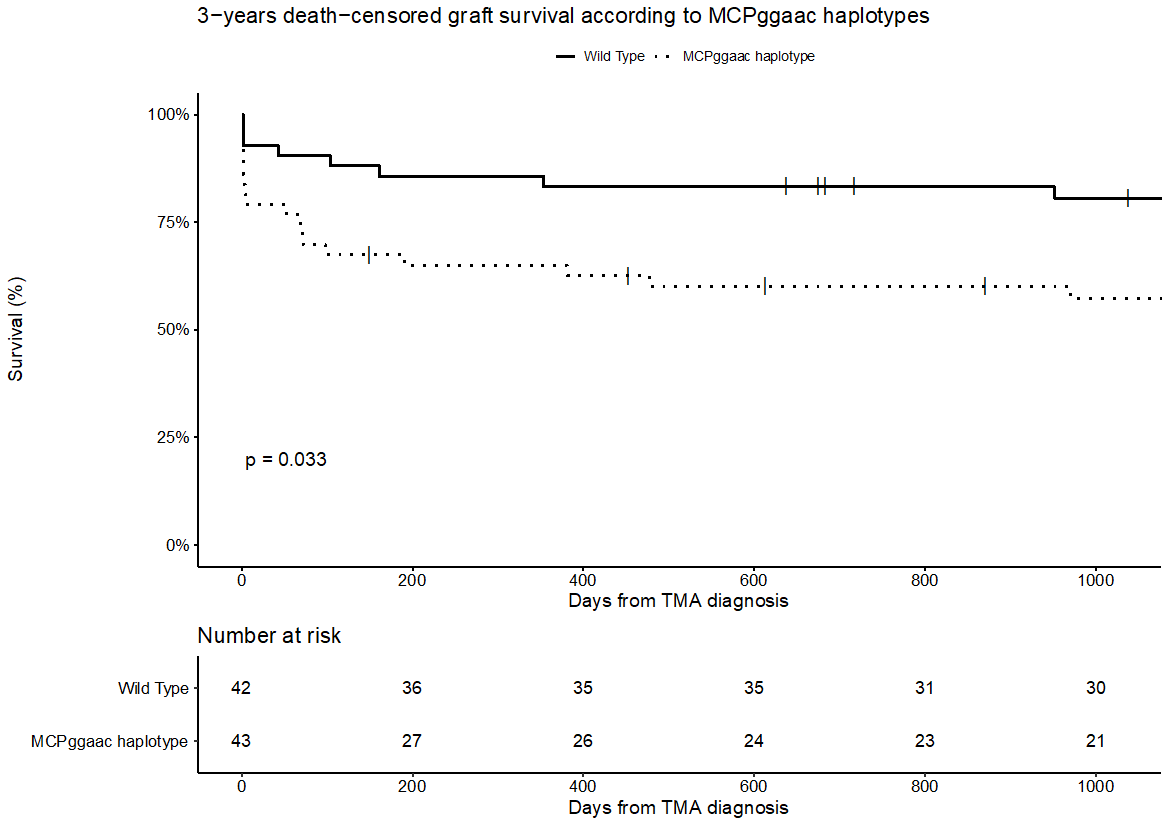
*Methods: Direct Sanger sequencing was performed in 90 KTR with de novo TMA and 90 corresponding donors on selected regions involving previously described variations in CFH (promoter, exons 9, 14, 19), CD46 (promoter, exon 10), C3 (exons 3, 9) and CFB (exon 2) genes, that have a functional effect or confer a risk for aHUS. Presence of the CFH H3 and MCPggaac risk haplotypes was deduced from genotype data of the variations identified in CFH and CD46. Additionally, 37 recipients of paired kidneys who did not develop TMA were analyzed for MCPggaac haplotype. Three-years death-censored graft survival was assessed using Kaplan-Meier and Cox regression models.
*Results: The distribution of haplotypes in all groups was in the Hardy-Weinberg equilibrium and there was no clustering of haplotypes in any group. In the TMA group, we found that MCPggaac haplotype carriers were at significantly higher risk of graft loss compared to the wild type carriers (57.4% vs. 77.9% death-censored graft survival in 3 years, Figure 1). Worse 3-years death-censored graft survival was associated with longer cold ischemia time (HR 1.21, 95% CI 1.07 – 1.37, p = 0.002), retransplantation status (HR 4.14, 95% CI 1.22 – 14.1, p = 0.02), and recipients´ MCPggaac haplotype (HR 3.24, 95% CI 1.27 – 8.27, p = 0.01) in the multivariable Cox regression model. There was no association between donors’ haplotypes and kidney graft survival. Similarly, there was no effect of MCPggaac haplotype on 3-years graft survival in recipients of paired kidneys who did not develop TMA after transplantation.
*Conclusions: Kidney transplant recipients carrying MCPggaac haplotype who develop de novo TMA are at increased risk of premature graft loss. Therefore, those patients might benefit from therapeutic strategies based on complement inhibition.
To cite this abstract in AMA style:
Petr V, Csuka D, Hruba P, Szilágyi Á, Prohászka Z, Viklicky O. Recipient MCPggaac Haplotype is Associated with Poor Graft Survival in Recipients with De Novo Thrombotic Microangiopathy [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/recipient-mcpggaac-haplotype-is-associated-with-poor-graft-survival-in-recipients-with-de-novo-thrombotic-microangiopathy/. Accessed February 6, 2026.« Back to 2022 American Transplant Congress