Transplant Glomerulopathy in the Absence of Donor-specific HLA Antibodies: Risk Factors, Histopathological Features and Graft Outcome
Microbiology, Immunology and Transplantation, KU Leuven, Leuven, Belgium
Meeting: 2021 American Transplant Congress
Abstract number: 319
Keywords: Biopsy, HLA antibodies, Kidney transplantation, Major histocompatibility complex (MHC)
Topic: Clinical Science » Kidney » Kidney Chronic Antibody Mediated Rejection
Session Information
Session Name: Kidney Antibody Mediated Rejection
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 8, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:40pm-4:45pm
Presentation Time: 4:40pm-4:45pm
Location: Virtual
*Purpose: Transplant glomerulopathy (TG) is established as a hallmark of chronic antibody-mediated rejection in kidney transplant patients with donor-specific HLA antibodies (HLA-DSA). The clinical importance of TG in the absence of HLA-DSA is not well established.
*Methods: Patients who underwent kidney transplantation between 2004-2013 were included in this study (N=954 with 3744 biopsies). We investigated the risk factors, histopathological appearance and prognosis of cases with TG in the absence of HLA-DSA, compared to cases of TG with HLA-DSA, and we evaluated the impact of the PIRCHE-II score and eplet mismatches, determined using high-resolution HLA genotyping, on TG development.
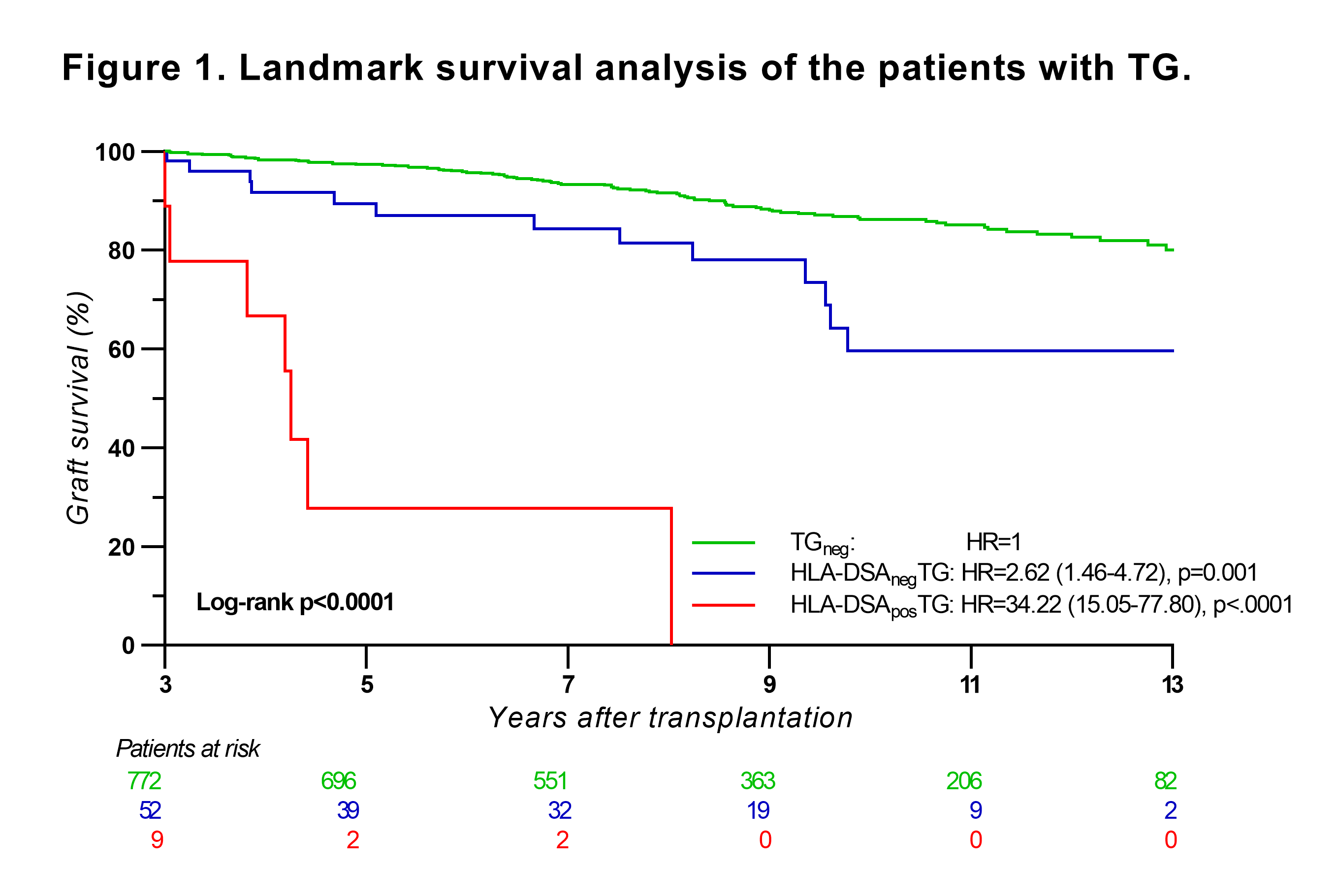
*Results: In this cohort, 98 patients (10.3%) developed TG, on average at 3.2 years posttransplant. At the time of TG, 23 patients (23.5%) had persistent pretransplant or de novo HLA-DSA (HLA-DSAposTG group), while 75 patients (76.5%) were HLA-DSA negative (HLA-DSAnegTG). Only HLA-DSA were identified as risk factor for TG development; HLA molecular mismatches, eplet mismatches and PIRCHE-II scores did not associate with TG. The HLA-DSAnegTG biopsies had less interstitial inflammation, less glomerulitis and less C4d deposition in peritubular capillaries compared to the HLA-DSAposTG biopsies. While graft function was comparable between the two groups, HLA-DSAposTG was associated with a higher risk of graft failure compared to HLA-DSAnegTG (HR=3.84; 95%CI 1.94-7.59; p=0.0001). Landmark analysis at 3-year post-transplant showed that HLA-DSAnegTG patients still had an increased risk of graft failure compared to TG-negative patients (HR=2.62; 95%CI 1.46-4.72; p=0.001).
*Conclusions: In conclusion, TG often occurs in the absence of HLA-DSA, independently of HLA molecular mismatches, and represents a different phenotype with less concomitant inflammation and better graft survival compared to TG developed in the presence of HLA-DSA.
To cite this abstract in AMA style:
Senev A, Loon EVan, Emonds M, Naesens M. Transplant Glomerulopathy in the Absence of Donor-specific HLA Antibodies: Risk Factors, Histopathological Features and Graft Outcome [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/transplant-glomerulopathy-in-the-absence-of-donor-specific-hla-antibodies-risk-factors-histopathological-features-and-graft-outcome/. Accessed February 7, 2026.« Back to 2021 American Transplant Congress