Liver Dysfunction Following Lung Transplantation
E. J. Hyzny1, E. G. Chan1, J. P. Ryan1, T. Harano1, M. R. Morrell2, P. G. Sanchez1
1Cardiothoracic Surgery, University of Pittsburgh School of Medicine, Pittsburgh, PA, 2Pulmonary, Allergy and Critical Care Medicine, University of Pittsburgh Medical Center, Pittsburgh, PA
Meeting: 2021 American Transplant Congress
Abstract number: 196
Keywords: Graft failure, Liver, Lung transplantation, Outcome
Topic: Clinical Science » Lung » Lung: All Topics
Session Information
Session Name: When Opportunity Knocks... Identifying Interventions to Optimize Lung Transplant Outcomes
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:35pm-6:40pm
Presentation Time: 6:35pm-6:40pm
Location: Virtual
*Purpose: To describe the incidence and risk factors for postoperative hepatic dysfunction (POHD) following lung transplantation (LT) and long-term outcomes for these patients.
*Methods: We performed retrospective analysis of 1261 adult LT recipients performed at our center between 1/1/2007- 12/1/2019. Patients were excluded for re-do LT or concurrent solid organ transplantation. POHD was defined by ICD-9 code designation. Chi-square analysis was performed for categorical variables and Mann Whitney U tests for continuous variables. Survival curves were estimated using Kaplan-Meier and log-rank test analysis.
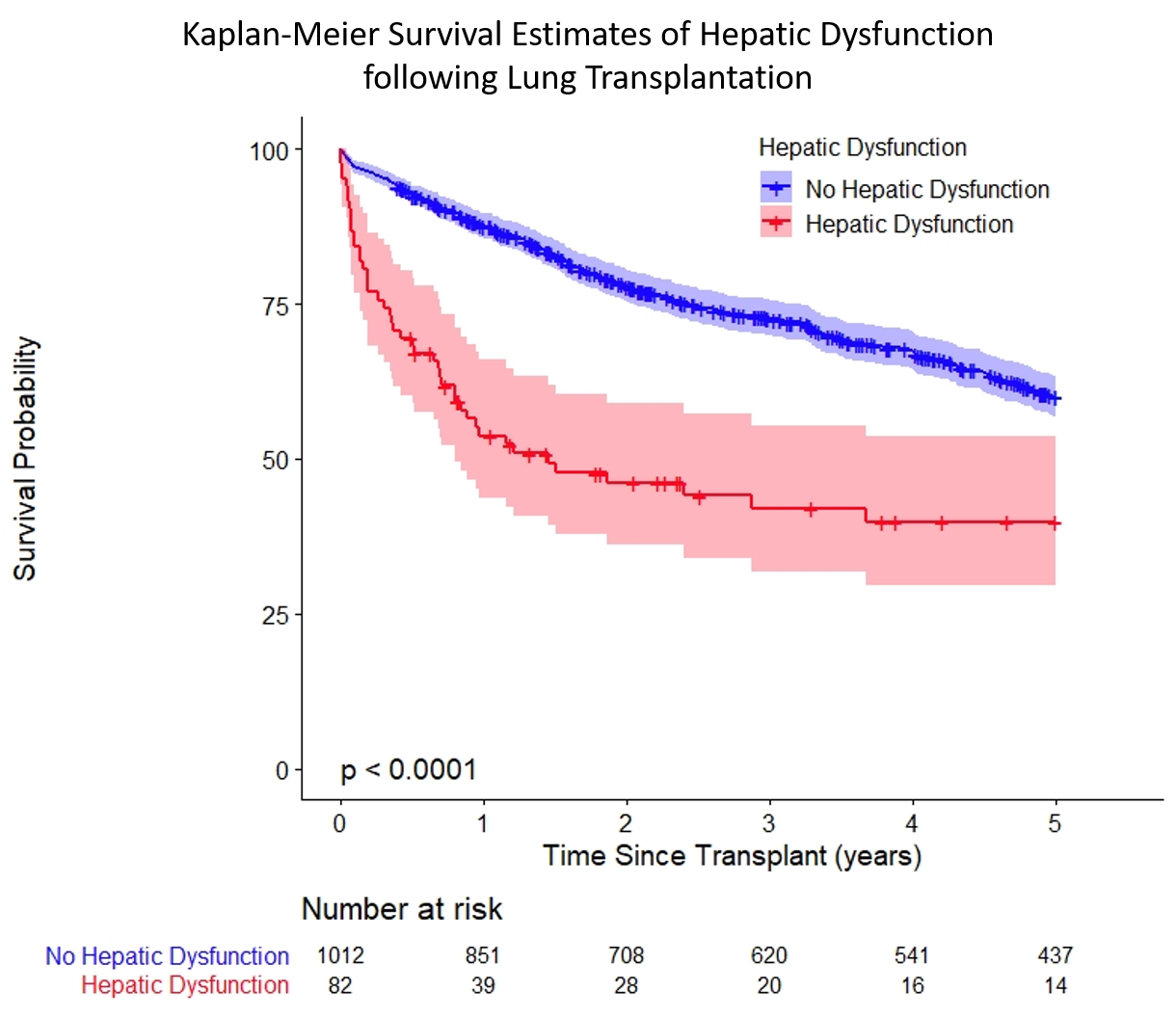
*Results: Out of the 1,094 primary lung transplants included, 82 (8.1%) developed POHD following LT. Predictors of POHD included a preoperative history of cirrhosis or portal hypertension (OR:22.13 (CI:5.19-94.40), p<0.001). Right upper quadrant ultrasonography (RUQ-US), performed in 112 (10.3%) patients for high preoperative suspicion of liver disease, was a significant predictor for POHD (OR: 2.73 (CI:1.55-4.80), p<0.001). Transplant diagnoses associated with obtaining preoperative RUQ-US due to clinical suspicion of preoperative liver dysfunction include pulmonary hypertension (p<0.001) and cystic fibrosis (p=0.01). Evidence of fibrosis on RUQ-US conveyed additional risk for POHD (OR:2.76 (CI:1.11-6.86, p=0.03). Other risk factors included use of intraoperative mechanical support (OR: 2.65 (CI: 1.62-4.25), p<0.001) and delayed chest incision closure (OR: 3.73 (CI:2.34-5.92), p<0.001). POHD was associated with longer ICU stay overall (10.5 vs 5 days, p < 0.001), increased duration requiring mechanical ventilatory support (15 vs 2.71 days, p < 0.001), and higher post-operative mortality (HR:11.23 (CI:6.34-19.88), p<.0001). Developing POHD was also associated with significantly lower long-term survival at 3 (p<0.001) and 5 years (p<0.001)(Figure 1).
*Conclusions: Following lung transplantation, hepatic dysfunction is a prevalent and morbid complication associated with high mortality. Additional studies are necessary to identify best treatment algorithm and practices to better avoid hepatic dysfunction in the postoperative setting following lung transplantation.
To cite this abstract in AMA style:
Hyzny EJ, Chan EG, Ryan JP, Harano T, Morrell MR, Sanchez PG. Liver Dysfunction Following Lung Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-dysfunction-following-lung-transplantation/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress