Risk of Histological Relapse in Patients with Monoclonal Gammopathy of Renal Significance after Kidney Transplantation
1Division of Nephrology and Hypertension, Mayo Clinic, Rochester, MN, 2Department of Internal Medicine, Dokuz Eylul University, Izmir, Turkey, 3Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN
Meeting: 2020 American Transplant Congress
Abstract number: C-064
Keywords: Graft failure, Histology, Monoclonal antibodies, Recurrence
Session Information
Session Name: Poster Session C: Kidney Complications: Non-Immune Mediated Late Graft Failure
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: There is increased recognition of Monoclonal Gammopathy of Renal Significance (MGRS) but data on kidney transplant (ktx)outcomes are lacking. We assessed KTX outcomes of patients with different MGRS phenotypes.
*Methods: We reviewed the charts of patients transplanted between 1990 and 2019 with MGRS as the cause of their native kidney disease and examined the recurrence rates, patient and allograft survival as well as response to treatments.
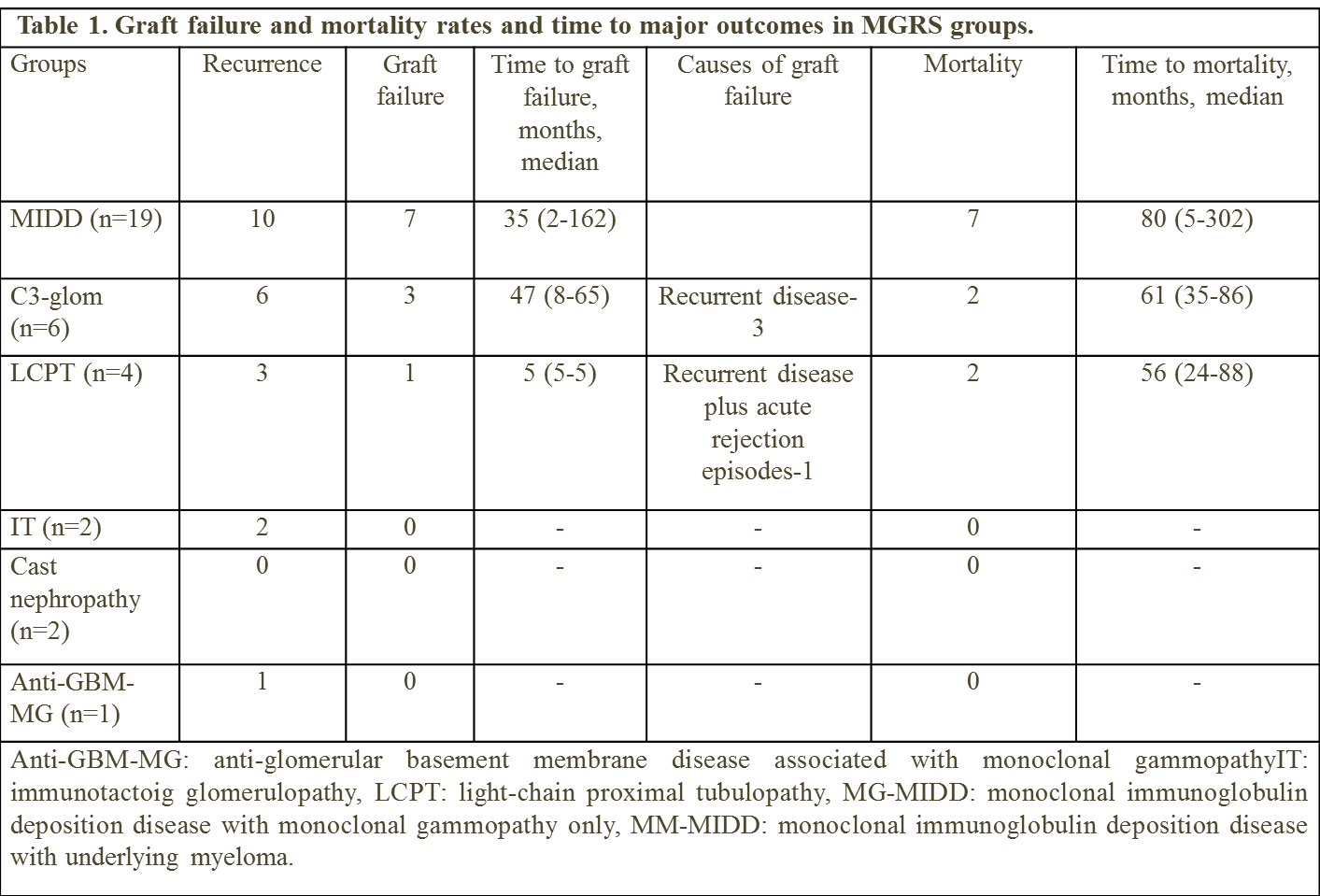
*Results: Thirty four patients(pts) with MGRS underwent KTX.Data presented in Table 1. Of the 19 pts in the monoclonal immunoglobulin deposition disease group, 11 were men (57.9%) . The median age at KTX was 58 (range, 19-68), 17 had LCDD and remaining 2 had HCDD. Histological relapse occurred in 10 pts (52.6%), 6(60.0%) of which were diagnosed by protocol biopsies. The majority had early findings of histologic relapse detected by immunofluorescence analysis alone. Graft failure was seen in 7 (36.8%), and mortality in 7 (36.8%). Median graft and patient survival were 162 and 117 months, respectively. Histological relapse was the main cause of graft loss in 4 subjects and contributed to graft failure in 1. Histological findings of recurrent disease were similar to the findings in native kidney biopsy in majority of the subjects. Of the 6 patients with C3-glomerulopathy with monoclonal gammopathy, median age was 57 (range, 39-73) and 5 were men (83.3%). All 6 had histological relapse at median 38 days (range, 11-126), all detected by clinical indication biopsies. Graft failure occurred in 3 (50.0%) and mortality in 2 (33.3%). In the light-chain proximal tubulopathy group (n=4), 3 patients were female (75.0%) and median age was 60 (40-68). Three patients had histological relapse after a median 68 (range, 25-423) days. Patients with cast nephropathy (n=2) had a complete remission of myeloma before the kidney transplantation and their post-transplant follow-up remained uneventful. Both of the patients with immunotactoid glomerulopathy and the patient with anti-GBM nephritis with monoclonal gammopathy had recurrence, but all had stable kidney function after clone-directed treatment.
*Conclusions: MGRS lesions differ significantly in terms of time to histological relapse and treatment responses. Protocol biopsies were crucial in capturing early recurrence especially in MIDD and can direct early therapy.
To cite this abstract in AMA style:
Bentall A, Heybeli C, Cosio FG, Ters MEl, Leung N, Alexander MP. Risk of Histological Relapse in Patients with Monoclonal Gammopathy of Renal Significance after Kidney Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/risk-of-histological-relapse-in-patients-with-monoclonal-gammopathy-of-renal-significance-after-kidney-transplantation/. Accessed February 5, 2026.« Back to 2020 American Transplant Congress