Impact of Chronic Changes on Preimplantation Biopsy (PBx) on Outcomes after Deceased Donor Kidney Transplantation (DDKTx)
Mayo Clinic, Phoenix, AZ
Meeting: 2020 American Transplant Congress
Abstract number: B-033
Keywords: Biopsy, Graft failure, Graft function, Kidney transplantation
Session Information
Session Name: Poster Session B: Kidney Deceased Donor Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The value of PBx is unclear. The aim of this study was to determine the prognostic value of chronic changes on PBx on graft survival and GFR after DDKTx.
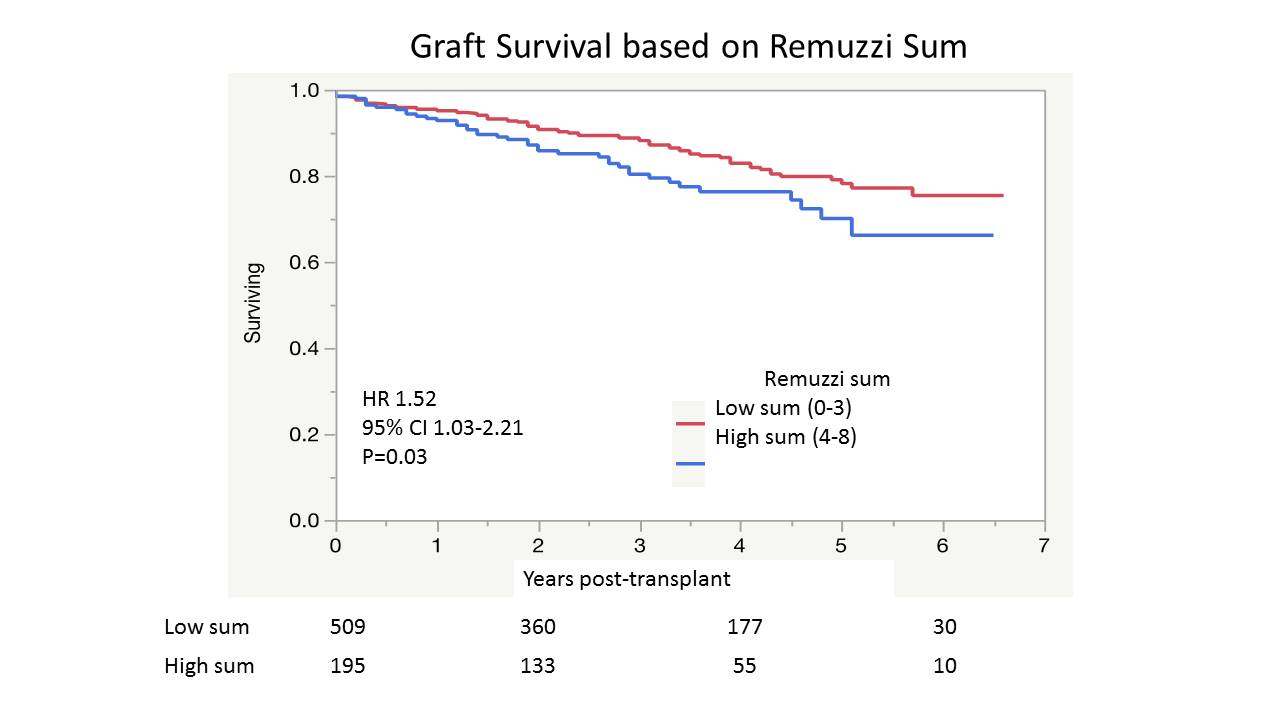
*Methods: All DDKTx recipients transplanted at our center between 1/2013 and 8/2018 were included. Pathology data from all PBx reports read at out center was collected. A modified Remuzzi(RU) score was used to quantify the chronic changes on PBx(glomerular sclerosis, interstitial fibrosis, arterial narrowing). The low RU sum group had a sum of 0-3(low sum) and the high RU sum group had a sum of 4-8(high sum). The outcomes were graft survival and eGFR at 1 year(yr).
*Results: The cohort size was 1,198. PBx was available in 758(63.3%). The median follow up for the cohort was 3.1 years. The median number of glomeruli in the PBx was 48(IQR 30-70). There was adequate data to calculate the RU score in 704 biopsies. The median RU sum score was 2(range 0-8) and 195(22.7%) had a high sum. The median(IQR) KDPI was 78(60-90) in the high sum and 53(34-75) in the low sum(P<.0001). Graft survival was lower in the high sum group(p=0.03).
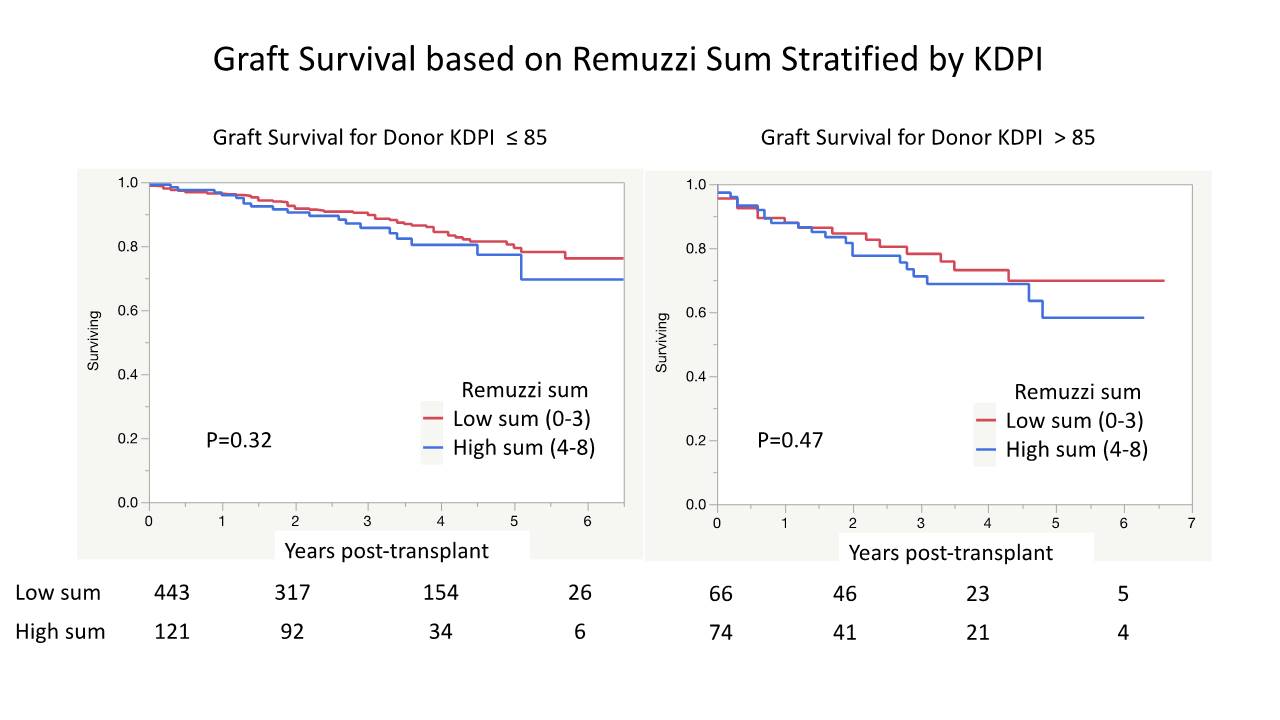
When stratified into two cohorts; KDPI>85 vs ≤85, the difference in graft survival was no longer apparent.
In a Cox model including the RU sum and the KDPI as a continuous variable, the high sum group was not a risk factor for graft survival(1.20, 95% CI 0.80-1.79). The eGFR at 1 yr was lower and the % with eGFR <30 at 1 yr was higher in the high sum group in the cohort with donor KDPI≤85. This difference was not as apparent in the cohort with donor KDPI>85 (table).
| KDPI<85 | KDPI<85 | KDPI>85 | ||||
| Low sum | High sum | p | Low sum | High sum | p | |
| eGFR 1 yr | 58.3 (20.3) | 49.7 (17.8) | 0.0002 | 42.0 (14.3) | 38.2 (12.9) | 0.21 |
| eGFR<30 (%) | 6.1 | 12.6 | 0.047 | 22.0 | 27.3 | 0.57 |
*Conclusions: Chronic changes on PBx correlated with lower mid-term graft survival and lower GFR at 1yr; however, after controlling for KDPI, RU sum no longer was a risk factor for graft survival. Our data suggests that PBx could be of value in the recipient selection for select KDPI ≤85 as a higher RU sum correlated with lower GFR at 1 yr.
To cite this abstract in AMA style:
Ninan J, Heilman R, Smith M, Harbell J, Nair SS, Jadloweic C, Khamash H, Moss A, Reddy KS. Impact of Chronic Changes on Preimplantation Biopsy (PBx) on Outcomes after Deceased Donor Kidney Transplantation (DDKTx) [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/impact-of-chronic-changes-on-preimplantation-biopsy-pbx-on-outcomes-after-deceased-donor-kidney-transplantation-ddktx/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress