A Multicenter Analysis of the Proportion and Pattern of Unexplained HLA Antibodies in Kidney Recipients without a History of Sensitization
1Medicine, Division of Nephrology, University of British Columbia, Vancouver, BC, Canada, 2Pathology, Emory University, Atlanta, GA, 3Pathology, Dalhousie University, Halifax, NS, Canada, 4Nephrology, Dalhousie University, Halifax, NS, Canada, 5Pathology, University of British Columbia, Vancouver, BC, Canada, 6Immunohaematology and Blood Transfusion, Leiden University Medical Center, Leiden, Netherlands, 7Nephrology, Emory University, Atlanta, GA
Meeting: 2020 American Transplant Congress
Abstract number: A-292
Keywords: Histocompatibility, HLA antibodies, HLA antigens, Multicenter studies
Session Information
Session Name: Poster Session A: Histocompatibility and Immunogenetics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Previous studies report a high prevalence of unexplained antibody reactivities on the single antigen bead (SAB) test. In a contemporary multicenter cohort of non-sensitized kidney recipients, our aim was to analyze the proportion and pattern of unexplained HLA antibodies and to quantify their impact on access to transplant.
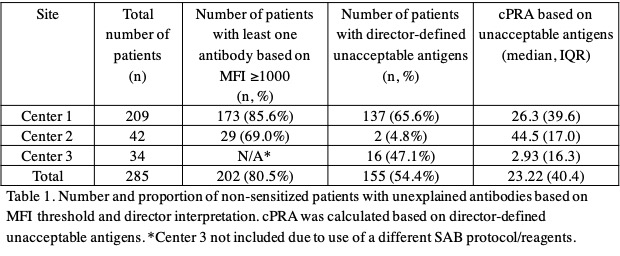
*Methods: OL SAB data from 285 non-sensitized patients from 3 US-Canadian centers were analyzed. Centers 1 and 2 utilized comparable SAB reagents/protocols, enabling comparison of the proportion of patients with HLA reactivities based on MFI ≥1000. The proportion of patients with director-defined unacceptable antigens and their associated cPRA was examined in all 3 centers.
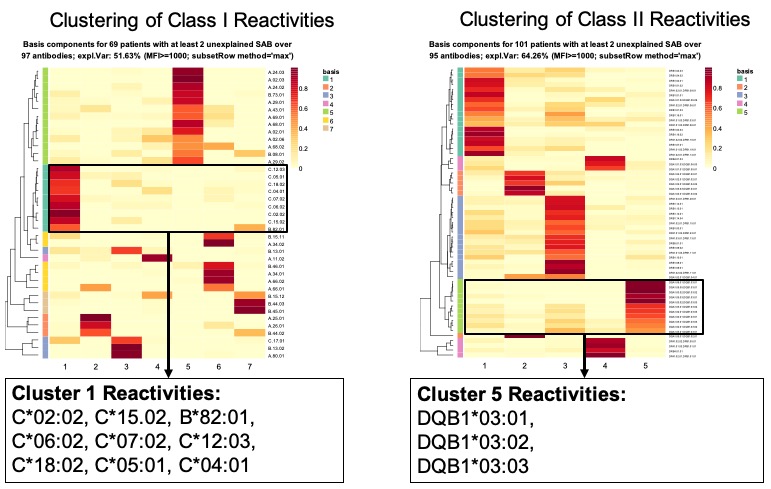
*Results: The majority of patients (n=202/251) had evidence of at least 1 reactivity based on MFI threshold ≥1000 (HLA-A: 13.3%, B: 17.9%, C: 8.1%, DR: 19.6%, DQ: 17.4%, DP: 23.7%), with 23% having a single, and the remaining having multiple antibodies. Unsupervised machine clustering identified distinct reactivity patterns in class I and II (Fig 1), some of which were shared between patients from different centers. Despite similarities in MFI-defined HLA specificities, significant differences were observed in the determination of unacceptable antigens between centers, leading to a differential impact on access to transplant (Table 1).
*Conclusions: The majority of non-sensitized kidney recipients showed evidence of unexplained reactivities on the SAB which can affect access to transplant. Further work is required to determine the etiology and relevance of spurious HLA reactivities not explained by clinical history.
To cite this abstract in AMA style:
Lan J, Gill JS, Gebel HM, Bray RA, Liwski R, Vinson A, Greenshields A, Dobrer S, Gunther O, Sherwood K, Claas FH, Heidt S, Karahan G, Gill J, Gill M, Varyani U, Jindal P, Keown P. A Multicenter Analysis of the Proportion and Pattern of Unexplained HLA Antibodies in Kidney Recipients without a History of Sensitization [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/a-multicenter-analysis-of-the-proportion-and-pattern-of-unexplained-hla-antibodies-in-kidney-recipients-without-a-history-of-sensitization/. Accessed February 23, 2026.« Back to 2020 American Transplant Congress