A Three-Decade Analysis of Pancreatic Adenocarcinoma Following Liver Transplantation
1Mayo Clinic, Rochester, MN, 2Mayo Clinic, Jacksonville, FL, 3Emory University, Atlanta, GA, 4Mayo Clinic Health System, Mankato, MN, 5Fox Chase Cancer Center, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: A-161
Keywords: Liver transplantation, Malignancy, Outcome, Pancreas
Session Information
Session Name: Poster Session A: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Liver transplant (LT) recipients are at risk of serious long term complications, including a higher risk of de novo malignancies compared to the general population. Data regarding the diagnosis of pancreatic adenocarcinoma (PC) following LT is limited. We aim to assess PC diagnosis as well as patient and tumor characteristics among those who developed PC post LT.
*Methods: 6847 adult patients 18 years and older from 3 academic centers of Mayo Clinic underwent LT between 1988 and 2018. A retrospective chart review was performed to assess the aim of the study.
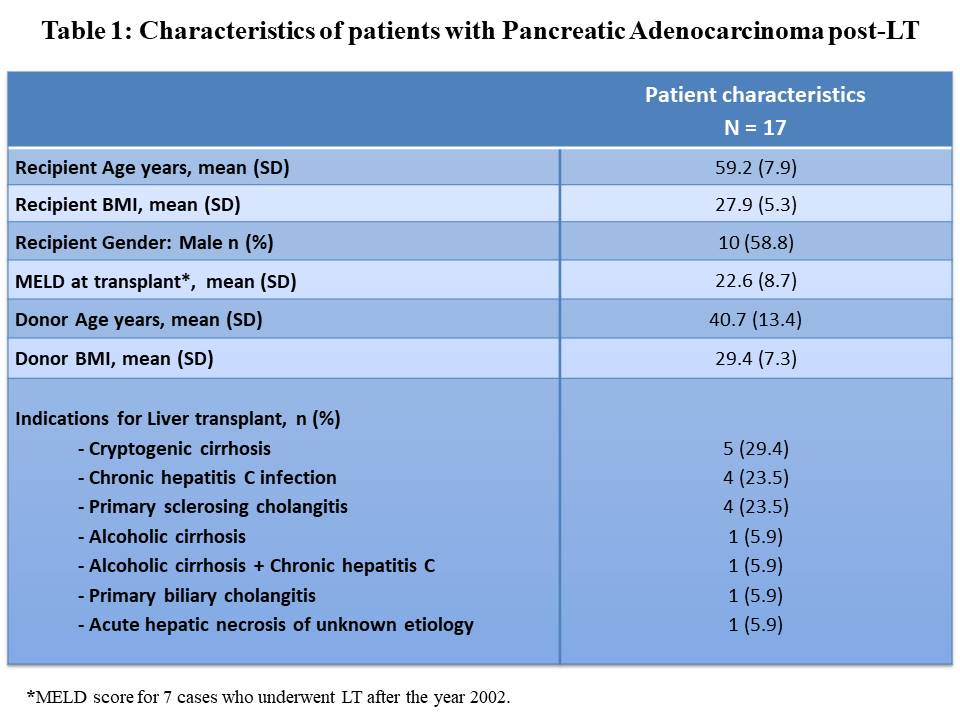
*Results: The 6847 patients were followed over 41,334 post-LT patient years. During follow up, 17 patients developed PC (mean age 59.2 years and 58.8% were males). Average one PC per 2431 post-LT patient years. 17.6% had a history of diabetes prior to LT, and 11.8% had hepatocellular carcinoma (HCC) at the time of LT (etiology of cirrhosis: cryptogenic and chronic hepatitis C in patients with HCC). Table 1 summarizes the patient characteristics.
The medical records regarding PC diagnosis and tumor characteristics were available for 6 patients. 83% (5/6) were diagnosed within the first 4 years following LT. All patients had negative contrast-enhanced cross sectional imaging within 1 year prior to LT, with no history of intrapapillary mucinous neoplasm (IPMN). Immunosuppression used following LT included: Tacrolimus or cyclosporin, mycophenolate mofetil and prednisone per protocol.
Time to PC diagnosis post-LT ranged between 5.2 months and 7.8 years. Time to death post-LT ranged between 6.2 months and 5.5 years in 5 patients. One patient who was diagnosed after 7.8 years is alive and underwent pancreatoduodenectomy.
The mean tumor size was 2.83 cm (SD±1.53). 83% (5/6) were in the pancreatic head/neck and 1 was in the tail of the pancreas. Liver metastasis was present at the time of diagnosis in 16.7% (1/6). 83.3% (5/6) underwent surgical resection and 2 of them were found to have a local invasion.
*Conclusions: Pancreatic adenocarcinoma is a rare but serious long-term complication with variable time to diagnosis post LT. In our experience, PC was more likely to present within the first 4 years post-LT, and metastasis or local invasion were likely to be present at the time of PC diagnosis. A history of diabetes was uncommon at the time of LT. Larger studies are needed to estimate the incidence and risk factors of PC following LT and evaluate the need for selective PC screening in LT recipients.
To cite this abstract in AMA style:
Mousa OY, Corral JE, Wijarnpreecha K, Shah R, Louwagie VS, Bartel MJ, Brahmbhatt B. A Three-Decade Analysis of Pancreatic Adenocarcinoma Following Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/a-three-decade-analysis-of-pancreatic-adenocarcinoma-following-liver-transplantation/. Accessed February 16, 2026.« Back to 2020 American Transplant Congress