Eosinophils Maintain Lung Allograft Tolerance by Sequestering CD8+ T Cells in Bronchial Associated Lymphoid Tissue
1Department of Surgery, University of Virginia, Charlottesville, VA, 2Department of Surgery, Washington University in St. Louis, St. Louis, MO
Meeting: 2020 American Transplant Congress
Abstract number: 626
Keywords: Eosinophils, Lung transplantation, T cells, Tolerance
Session Information
Session Name: Tolerance / Immune Deviation
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:39pm-3:51pm
Presentation Time: 3:39pm-3:51pm
Location: Virtual
*Purpose: It has been recently described that eosinophils can facilitate immunosuppression-mediated acceptance of murine lung allografts. But the role of eosinophils in long term maintenance of lung allograft integrity remains unknown.
*Methods: To investigate the role of eosinophils in long term allograft acceptance, we transplanted fully MHC-mismatched BALB/c (H2d) lung allografts to transgenic mice on a C57BL/6 background (H2b) where the diphtheria toxin receptor is selectively expressed in eosinophils based on eosinophil peroxidase-specific promoter (iPHIL mouse). Tolerance was induced using perioperative co-stimulatory blockade of the CD40-CD40L and CD28-CD80/86 pathways. Four weeks after engraftment eosinophils were depleted through administration of diphtheria toxin for two weeks and the grafts were analyzed by flow cytometry, histology, and immunohistochemistry.
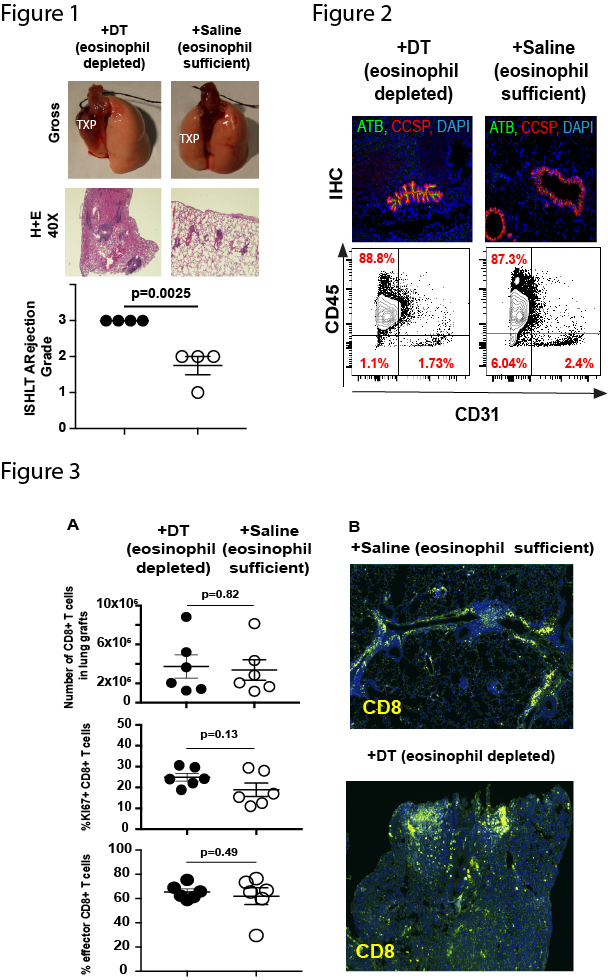
*Results: One month post engraftment eosinophils comprised <1% of all leucocytes. Despite low numbers their depletion result in gross and histologic rejection of the lung allograft (Figure 1). Further histologic and flow cytometric analysis revealed loss of small airways and flow cytometric loss of CD45-CD31- stromal cells such as CCSP+ Club cells (Figure 2 and data not shown). Flow cytometric analysis did not demonstrate and increase in T cell number or proliferation (as measured by KI67 upregulation) or effector differentiation (as measured by portion of CD44hiCD62Llow effector differentiation) (Figure 3a). Immunohistochemistry did demonstrate that with eosinophil depletion altered CD8+ T cell distribution within the lung graft. In eosinophil sufficient grafts CD8+ T cells were mostly localized to peribronchial associated lymphoid tissue while in eosinophil-deficient grafts CD8+ T cells localized throughout the lung parenchyma (Figure 3b).
*Conclusions: We now demonstrate that in addition to their role induction of tolerance eosinophils also play a critical role in maintenance of lung allograft acceptance. Unlike the case for early in the perioperative period, where eosinophils prevented T cell activation and proliferation, their delayed mechanism seems to involve a form of sequestration and prevention of the destruction of small airway stromal tissue. Our findings suggest that manipulation of eosinophils may offer therapeutic options for not just the establishment but maintenance of lung allograft tolerance.
To cite this abstract in AMA style:
Mei Z, Guo Y, Hata A, Banerjee A, Li D, Manafi A, Mahgoub B, Kreisel D, Gelman A, Krupnick AS. Eosinophils Maintain Lung Allograft Tolerance by Sequestering CD8+ T Cells in Bronchial Associated Lymphoid Tissue [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/eosinophils-maintain-lung-allograft-tolerance-by-sequestering-cd8-t-cells-in-bronchial-associated-lymphoid-tissue/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress