Epithelial to Mesenchymal Transition: A Cellular Mediator of Ischemic Cholangiopathy after Liver Transplant
1VCUHealth, Richmond, VA, 2Department of Surgery, VCUHealth, Richmond, VA
Meeting: 2019 American Transplant Congress
Abstract number: B4
Keywords: Bile duct, Donors, non-heart-beating, Epithelial cells, Warm ischemia
Session Information
Session Name: Poster Session B: Ischemia Reperfusion & Organ Rehabilition
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Epithelial-to-mesenchymal transition (EMT) is a genetic reprogramming that causes epithelial cells to assume a migratory, mesenchymal phenotype, and it is induced by hypoxia. Ischemic cholangiopathy (IC), which is characterized by disappearance and fibrosis of the biliary system, may involve cholangiocyte EMT under donation after cardiac death (DCD) conditions. Our hypothesis was that DCD conditions will induce EMT in cholangiocytes.
*Methods: Primary cholangiocytes were exposed to warm ischemia and cold storage (WI+CS) or cold storage alone (CS) and rewarmed to simulate preservation injury. Fresh cholangiocytes served as controls (Table 1). Genetic, phenotypic, and morphologic evidence of EMT were assessed by qPCR, migration assays, immunocytochemistry (Table 2), and microscopy at 1, 7, 14, and 21 days post-reperfusion.
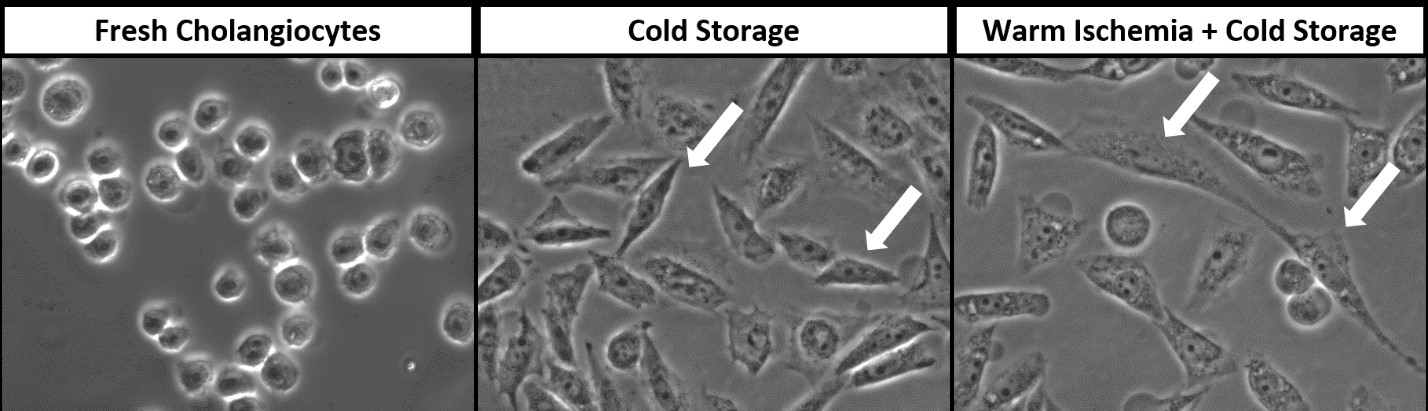
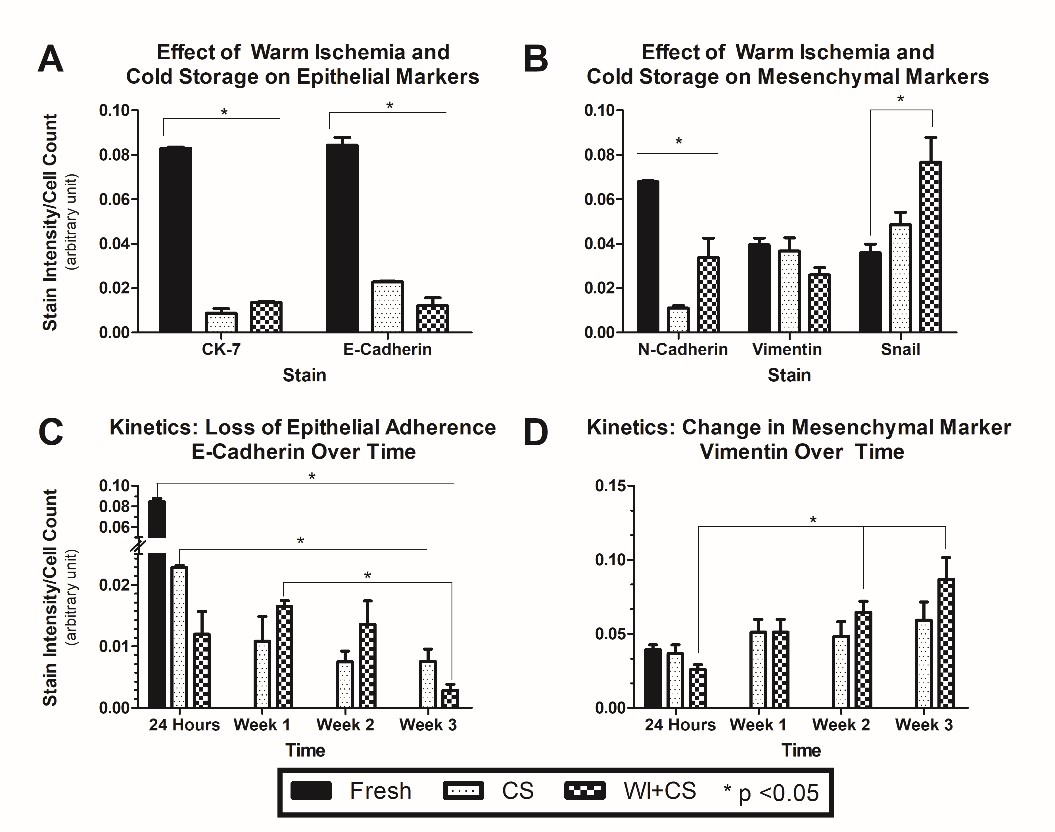
*Results: Warm ischemia caused increased migration through a collagen matrix up to 3 weeks after exposure to ischemia, relative to fresh cholangiocytes. Both the CS and WI+CS groups demonstrated a shift in morphology to fibroblast-like cells 24 hours after reperfusion (Figure 1). Both groups demonstrated a significant loss in expression of epithelial markers (Figure 2A). Only the WI+CS group demonstrated increased expression of the EMT-associated transcription factor, SNAIL (2B). E-cadherin expression continued to decrease over time in both groups (2C), while only the WI+CS group demonstrated a sustained increase in the mesenchymal marker, Vimentin (2D). The EMT-associated changes in protein expression mirrored changes in gene expression (qPCR).
*Conclusions: In conclusion, primary human cholangiocytes exposed to warm ischemia and cold storage displayed morphologic, genetic, and a phenotypic changes consistent with an EMT.
| Treatment Group | Storage Conditions | Reperfusion |
| Fresh cholangiocytes (negative control) | No ischemia | No reperfusion |
| Cold Storage (CS) | 24 hours cold ischemia: 4oC, 0% O2 | Reperfusion: 37oC, 5% CO2 +atmospheric air |
| Warm Ischemia + Cold Storage (WI+CS) | 1 hour warm ischemia: 37oC, 0% O2 24 hours cold ischemia: 4oC, 0% O2 | Reperfusion: 37oC, 5% CO2 +atmospheric air |
| Pathway | ICC Marker | Cellular Function |
| Loss of epithelial cell adhesion | E-Cadherin | Belt desmosome associated with cell-cell adherence |
| Cytokeratin-7 (CK-7) | Intracytoplasmic structural protein found in epithelial cells | |
| Change in transcriptional regulation | SNAIL | Transcriptional repressor of E-cadherin |
| Upregulation of mesenchymal markers | N-Cadherin | Mesenchymal adhesion molecule that promotes cell migration |
| Vimentin | Mesenchymal cytoskeletal protein |
Figure 1.
Figure 2.
To cite this abstract in AMA style:
Wickramaratne NA, Li R, Fyffe-Freil RC, Tian T, Mangino MJ. Epithelial to Mesenchymal Transition: A Cellular Mediator of Ischemic Cholangiopathy after Liver Transplant [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/epithelial-to-mesenchymal-transition-a-cellular-mediator-of-ischemic-cholangiopathy-after-liver-transplant/. Accessed February 14, 2026.« Back to 2019 American Transplant Congress