Elevated Urinary Injury Biomarkers in Deceased Donors Are Not Associated with Long-Term Kidney Transplant Outcomes
DDS Consortium, Baltimore, MD
Meeting: 2019 American Transplant Congress
Abstract number: A153
Keywords: Graft survival, Kidney transplantation, Renal injury, Urinalysis
Session Information
Session Name: Poster Session A: Biomarkers, Immune Monitoring and Outcomes
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: In the United States, over 90,000 people are on the kidney transplant waiting list and could benefit from more donor organs. Kidneys from deceased-donors with clinical Acute Kidney Injury (AKI) have similar long-term allograft survival as non-AKI donor kidneys. However, organ procurement organizations discard AKI donor kidneys at a higher rate than non-AKI donor kidneys. Better tools that accurately predict recipient outcomes can improve allocation decisions. Urinary injury biomarkers are sensitive markers of structural kidney damage to nephrons. In this study, we evaluated the role of urinary injury biomarkers in predicting long-term kidney transplant outcomes.
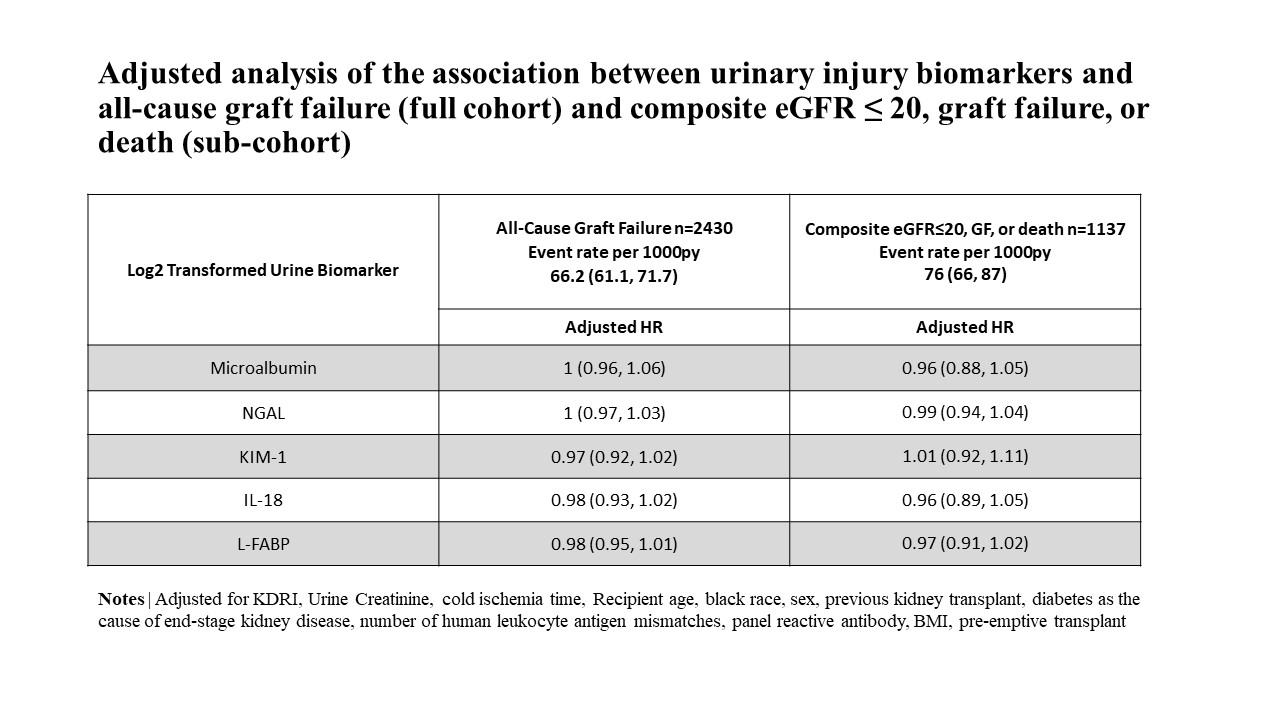
*Methods: In the 2010-2013 multicenter Deceased Donor Study of 2430 kidney transplant recipients from 1298 donors, we assessed the association between donor urine injury biomarkers and recipient all-cause graft failure (all-cause mortality, return to dialysis, or re-transplantation) and death-censored graft failure using Cox proportional hazard models. We measured donor urine concentrations of the following biomarkers: microalbumin, neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1 (KIM-1), IL-18, and liver-type fatty acid binding protein (L-FABP). Through chart review of a sub-cohort of 1137 recipients, we determined associations between donor urinary biomarkers and a 3-year composite outcome of all-cause graft failure or estimated glomerular filtration rate (eGFR) <=20 mL/min/1.73m2. In sub-analysis, we observed posttransplant outcomes among patients with subclinical AKI – defined as elevated urinary injury biomarkers in patients without AKI.
*Results: Risk of all-cause graft failure and death-censored graft failure in the full cohort or 3-year composite all-cause graft failure or eGFR <= 20 in the sub-cohort did not vary with donor urinary injury biomarker concentrations, after adjusting for donor, transplant, and recipient characteristics (Table). In stratified analysis, subclinical donor injury in patients without AKI was also not significantly associated with long-term allograft survival.
*Conclusions: Prior results show donor AKI kidneys yielded similar long-term allograft function versus donor kidneys without AKI. This study suggests donor urinary injury biomarkers are not associated with higher graft failure or reduction in eGFR. Cautious utilization of donor AKI kidneys may expand the deceased-donor kidney pool.
To cite this abstract in AMA style:
Koyawala N, Hall IE, Jia Y, Mansour SG, Reese PP, Thiessen-Philbrook HR, Akalin E, Bromberg JS, Doshi MD, Harhay MN, Mohan S, Muthukumar T, Schroppel B, Singh P, Weng FL, Parikh CR. Elevated Urinary Injury Biomarkers in Deceased Donors Are Not Associated with Long-Term Kidney Transplant Outcomes [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/elevated-urinary-injury-biomarkers-in-deceased-donors-are-not-associated-with-long-term-kidney-transplant-outcomes/. Accessed February 1, 2026.« Back to 2019 American Transplant Congress