The Impact of Portal Flow after Reperfusion on Graft Outcomes after Deceased Donor Liver Transplantation
General Surgery, Digestive Disease & Surgery Institute, Cleveland Clinic, Cleveland Clinic, Cleveland, OH
Meeting: 2019 American Transplant Congress
Abstract number: 227
Keywords: Graft function, Graft survival, Liver transplantation
Session Information
Session Name: Concurrent Session: Liver Transplant Complications and Retransplantation I
Session Type: Concurrent Session
Date: Monday, June 3, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:54pm-3:06pm
Presentation Time: 2:54pm-3:06pm
Location: Ballroom A
*Purpose: The impacts of intraoperative portal flow (PF) on graft outcomes after living donor liver transplantation have been studied well, however, its impact on graft outcomes after deceased donor whole liver transplantation (DDLT) remains unclear. This study aimed to investigate the impact of PF on graft and recipient outcomes after DDLT.
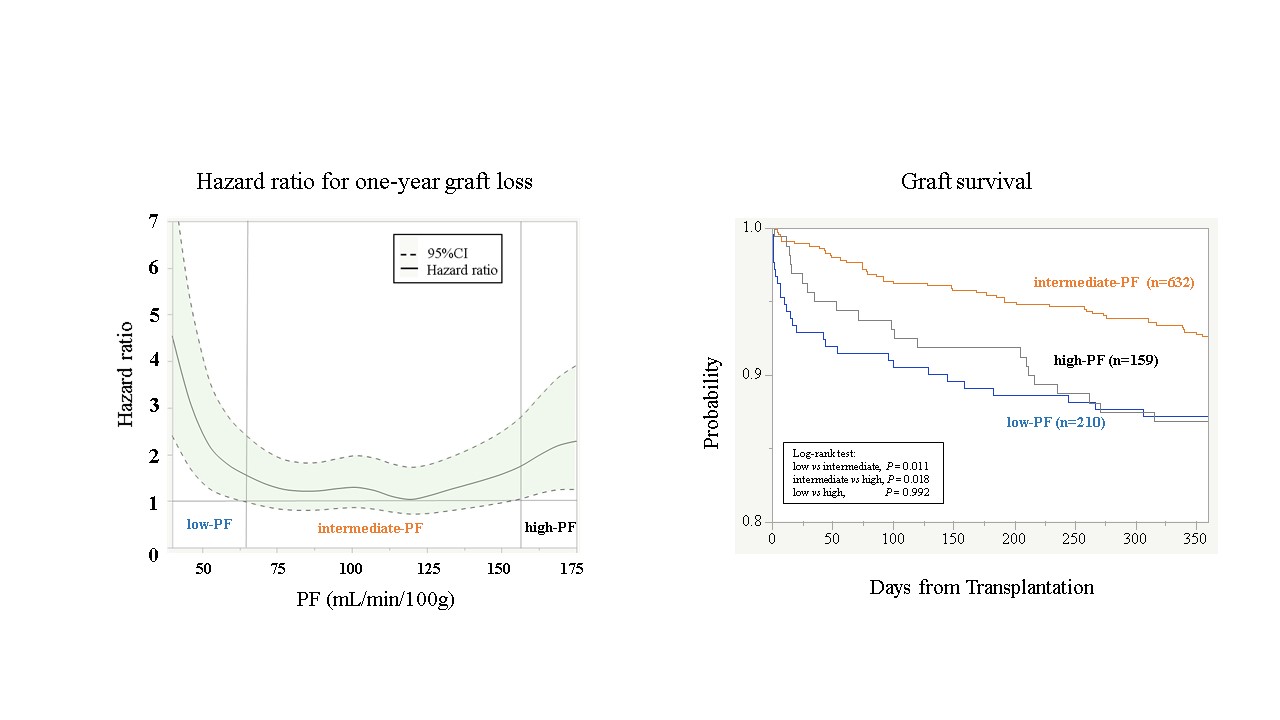
*Methods: We conducted a retrospective analysis of 1,001 patients who underwent DDLT at our institution. The patients were divided into three groups according to hazard ratio for one-year graft loss at each PF value; the low-PF group, the intermediate-PF group and the high-PF group. The graft and recipient outcomes were compared between the three groups.
*Results: PF showed bidirectional impacts on one-year graft survival. The patients in the low-PF group (PF < 65 mL/min/100g, n = 210) and the high-PF group (PF > 155 mL/min/100g, n = 159) showed significantly poorer graft and patient survival compared with those in the intermediate-PF group (PF > 65 mL/min/100g and < 155 mL/min/100g, n = 632). The frequency of primary non-function and early allograft dysfunction in the low-PF group were higher than the intermediate-PF group (P = 0.014 and P < 0.0001, respectively). Intraoperative hepatic artery flow of patients in the high-PF group was lower than the-intermediate groups (P = 0.025). The cumulative incidence rates of hepatic artery thrombosis and biliary complications in the high-PF group were significantly higher than in the-intermediate group (P = 0.028 and P = 0.017, respectively).
*Conclusions: Sufficient PF might be essential for favorable graft function, but excessive PF could be a risk factor for the development of hepatic artery thrombosis by decreasing HAF, resulting in early graft loss.
To cite this abstract in AMA style:
Matsushima H, Sasaki K, Fujiki M, Uso TDiago, Eghtesad B, Aucejo F, Kwon C, Miller C, Quintini C, Hashimoto K. The Impact of Portal Flow after Reperfusion on Graft Outcomes after Deceased Donor Liver Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-portal-flow-after-reperfusion-on-graft-outcomes-after-deceased-donor-liver-transplantation/. Accessed February 18, 2026.« Back to 2019 American Transplant Congress