Improved Transplant Outcomes in Ischemia-Free Liver Transplantation: A Report of the First 30 Cases
Organ Transplant Center, the First Affiliated Hospital of SYSU, Guangzhou, China
Meeting: 2019 American Transplant Congress
Abstract number: 97
Keywords: Graft function, Ischemia, Kidney/liver transplantation, Liver
Session Information
Session Name: Concurrent Session: Non-Organ Specific:Organ Preservation/Ischemia Reperfusion Injury
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:42pm-2:54pm
Presentation Time: 2:42pm-2:54pm
Location: Room 209
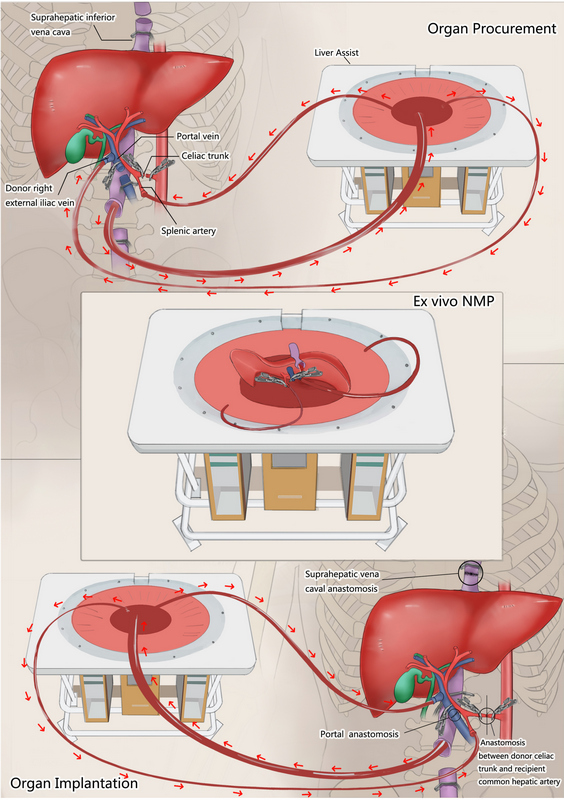
*Purpose: We developed a novel procedure called ischemia-free liver transplantation (IFLT) to bridge liver grafts from donors to recipients without cessation of blood supply. Herein, we report the clinical outcomes of the first 30 cases of IFLT in human.
*Methods: IFLT involves innovative surgical techniques and the use of normothermic machine perfusion to enable a continuous oxygenated blood supply to donor livers during procurement, preservation and implantation.
In this prospective, non-randomized controlled study, 30 donor livers were transplanted in the IFLT group. Livers that were transplanted using a conventional procedure during the same period were treated as controls. The primary end-point was the incidence of early allograft dysfunction (EAD).
*Results: During the operation, the body temperature and mean arterial pressure were more stable and the incidence of post-reperfusion syndrome was much lower in IFLT. Of the 30 patients in the IFLT group, 1 (3%) had EAD, compared with 47 of 89 (53%) patients in the control group (absolute risk difference, -46 percentage points; 95% confidence interval [CI], -65 to -25). The peak aspartate aminotransferase (365 versus 1551 U/L, P<0.001) and alanine aminotransferase (169 versus 660 U/L, P<0.001) serum levels were much lower in the IFLT group. The total bilirubin level on day 7 post-transplantation was lower in the IFLT group than in the control group (2.3 versus 5.7 mg/dL, p<0.001). No PNF occurred in the IFLT group, while there were 5 cases of PNF (6%) in the control group. The patient and graft survival were comparable between the two groups.
| EAD | 1(3.3%) | 47(53%) | <0.001 |
| Peak AST (U/L) within 7 days | 365(151-4112) | 1551(384-9951) | <0.001 |
| Peak ALT (U/L) within 7 days | 169(60-3474) | 660(86-6426) | <0.001 |
| Tbil (mg/dL) on day 7 | 2.3(0.8-11.9) | 5.7(0.6-38.2) | <0.001 |
| INR | 1.2(1.02-1.51) | 1.11(0.96-1.84) | 0.04 |
| PNF | 0 | 5(6%) | 087 |
| Non-anastomosis biliary stricture | 0 | 8(9%) | 0.32 |
| Need for renal replacement treatment | 1(3.3%) | 20(22%) | 0.43 |
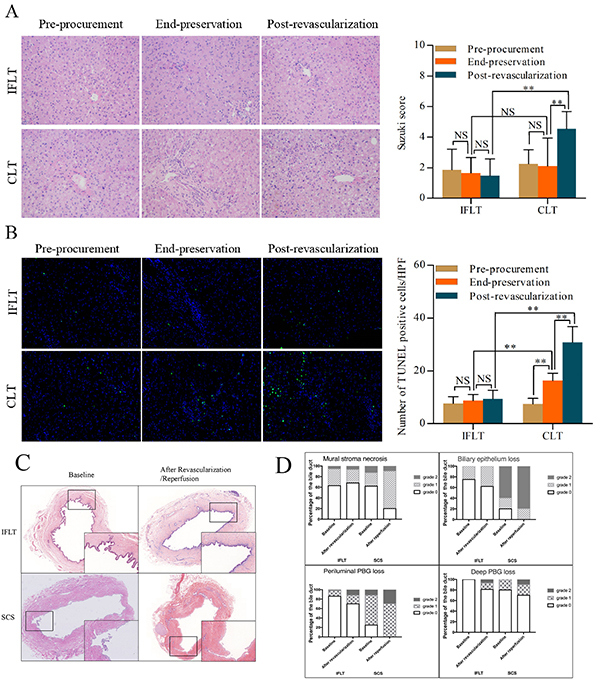
The pathological studies revealed minimal injury of hepatocytes and biliary epithelium during IFLT. The bile with good quality was continually produced throughout procurement, preservation and implantation in IFLT. There was no non-anastomosis biliary stricture in the IFLT group, compared with 8 cases in the control group (9%). Histological analysis of IFLT allograft biopsies and TUNEL showed a minimal injury to the liver tissues and bile duct.
*Conclusions: IFLT provides an innovative approach to avoid graft ischemia-reperfusion injury and can therefore optimize post-transplant outcomes and maximize organ utilization.
To cite this abstract in AMA style:
He X, Guo Z, Ju W, Zhao Q, Huang S, Yang J, Wang L, Tang Y, Zhang Z, Zhu Z, Yang L, Zhu Y, Gong F, Cai C, Huang W, Chen G, Chen M, Ji F, Han M, Hu A, Wu L, Ma Y, Wang D, Huang J, Li X. Improved Transplant Outcomes in Ischemia-Free Liver Transplantation: A Report of the First 30 Cases [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/improved-transplant-outcomes-in-ischemia-free-liver-transplantation-a-report-of-the-first-30-cases/. Accessed February 21, 2026.« Back to 2019 American Transplant Congress