Mechanisms of Vascularized Bone Marrow Graft Protection of Vascularized Composite Allografts
Surgery, University of Maryland, Baltimore, MD.
Meeting: 2018 American Transplant Congress
Abstract number: 286
Keywords: Graft survival, Microchimerism, Primates, Tolerance
Session Information
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: Room 303
Background Co-transplantation of vascularized bone marrow (VBM) promotes vascularized composite allograft (VCA) survival with standard immunosuppression in a non-human primate (NHP) model. We investigated mechanisms of immunomodulation by comparing VCA survival following donor bone marrow cell (BMC) infusion, donor and recipient conditioning strategies, and heterotopic VBM allografts to historical groups.
Methods Groups of 3-4 NHP received facial subunit VCA and immunosuppression of tacrolimus (Tac) and mycophenolate mofetil (MMF). Comparative groups VCA+VBM (n=4) and VCA no VBM (n=3) were from historical cohorts (Group 1 and 2, respectively). Group 3 received VCA without VBM and transfused donor BMC at 20x 106 cells/kg on d 1. Groups 4 and 5 received VCA+VBM with irradiated donor mandible (1.5 Gy) on d -1; Group 5 also received donor BMC transfusion on d 1. Group 6 underwent co-transplantation of heterotopic VBM and VCA without VBM. Group 7 received VCA+VBM after donor T cell depletion (TCD) with anti-thymocyte globulin (ATGAM, 50 mg/kg) on days -2, -1, and 0 to achieve CD3+ cell count <50/mm3. Group 8 recipients received ATGAM depletion as above, VCA+VBM, and a 21-d steroid taper. Banff classification was determined by histopathologic analysis. Chimerism was assessed by flow cytometry from peripheral blood and sampled tissues.
Results VCA+VBM treated with Tac/MMF demonstrated prolonged graft survival (p=0.05) and rejected only after immunosuppression was withdrawn compared to Groups 2-8 (mean survival 348d vs 36d).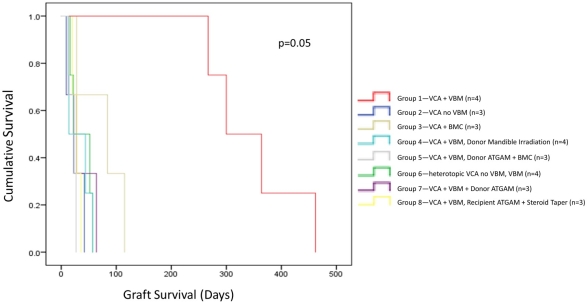 Endpoints were met secondary to Banff IV rejection and malignancy. Macrochimerism was only present in Group 1; remaining groups exhibited transient microchimerism.
Endpoints were met secondary to Banff IV rejection and malignancy. Macrochimerism was only present in Group 1; remaining groups exhibited transient microchimerism.
Conclusions The immunologic advantage of VBM on VCA graft survival is contingent on proximity of VBM to allograft. Donor conditioning nullifies this benefit and it is not reconstituted by donor BMC transfusion. Recipient TCD mirrors the early graft loss observed with donor TCD. Our data elucidate a mechanism for VCA graft survival that is mediated by locally acting, radiosensitive T cell populations and is dependent on the immunologic and structural niche of VBM.
CITATION INFORMATION: Buckingham E., Shockcor N., Hassanein W., Drachenberg C., Nam A., Bartlett S., Barth R. Mechanisms of Vascularized Bone Marrow Graft Protection of Vascularized Composite Allografts Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Buckingham E, Shockcor N, Hassanein W, Drachenberg C, Nam A, Bartlett S, Barth R. Mechanisms of Vascularized Bone Marrow Graft Protection of Vascularized Composite Allografts [abstract]. https://atcmeetingabstracts.com/abstract/mechanisms-of-vascularized-bone-marrow-graft-protection-of-vascularized-composite-allografts/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress
