Postoperative Serum Lactate Dehydrogenase Is a "Troponin-Like" Marker of Renal Transplant Distress.
UCSD Center for Transplantation, University of California at San Diego, San Diego, CA
Meeting: 2017 American Transplant Congress
Abstract number: A179
Keywords: Graft function, Kidney transplantation, Renal injury, Renal ischemia
Session Information
Session Name: Poster Session A: Kidney Complications I
Session Type: Poster Session
Date: Saturday, April 29, 2017
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall D1
Lactate dehydrogenase (LDH) is plentiful in renal tubular cells and is released during tubular injury or death. It increases for several days to 1500-2000 U/L after unilateral renal infarction. We measured serum LHD serially in the first post transplant week as a marker of renal distress in 60 sequential transplanted kidneys from living donors (LDKs) (n=20) , standard deceased donors (DDKs) (n=20), or donors after circulatory death (DCDKs) (n=20). All patients received thymoglobulin; DDKs and DCDks received pulsatile perfusion.
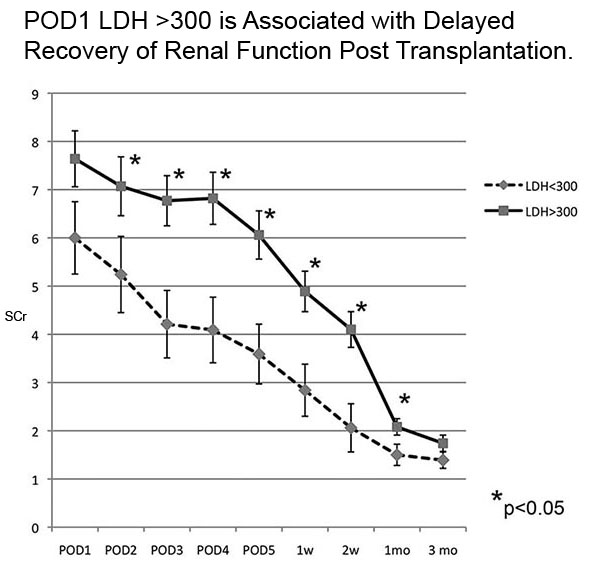
LDH was slightly higher on day 1 but varied little in the first post transplant week. It was lowest and usually normal (< 175 U/L) in LDKs, intermittently elevated in DDKs, and highest in DCDKs (figure 1). In deceased donors, higher LDH values were associated with delayed recovery, with a threshold of >300 U/L best differentiating grafts with slower improvement in serum creatinine (figure 2). Day 1 LDH was not influenced by hematocrit, platelet count, KDPI, or donor age. Not incuded were LDH values of 1500-2000 U/L in two patients wih major vascular complications, in one patient with HUS (with thrombocytopenia in all 3), and in one patient with 6 weeks of severely oliguric ATN that eventually resolved. With or without LDH "leak," the daily improvement in GFR in most cases was consistent with a resolving sublethal tubular injury, which was less severe than true tubular necrosis.
In summary, postoperative LDH was increased in proportion to expected ischemic stress in LD, DD and DCD kidneys. Such stress is usually transient and not severe enough to cause true ATN. Following serum LHD in transplanted kidneys may be analogous to measuring troponin to assess cardiac ischemia. Normal values are good prognostic signs, but major elevations suggest secondary pathology that will delay or prevent recovery.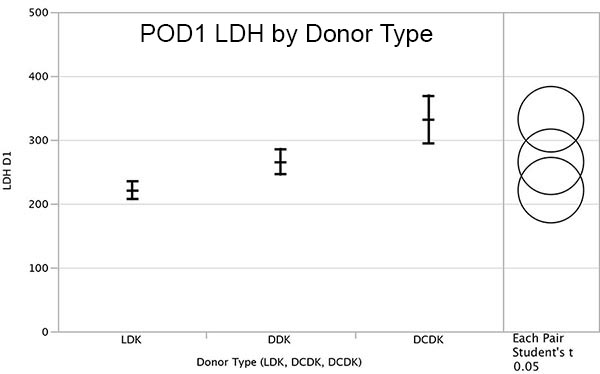
CITATION INFORMATION: Steiner R, Halldorson J. Postoperative Serum Lactate Dehydrogenase Is a "Troponin-Like" Marker of Renal Transplant Distress. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Steiner R, Halldorson J. Postoperative Serum Lactate Dehydrogenase Is a "Troponin-Like" Marker of Renal Transplant Distress. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/postoperative-serum-lactate-dehydrogenase-is-a-troponin-like-marker-of-renal-transplant-distress/. Accessed February 16, 2026.« Back to 2017 American Transplant Congress
