Waiting List Mortality of Liver Tumors
Division of Transplantation, Massachusetts General Hospital, Boston, MA
Meeting: 2020 American Transplant Congress
Abstract number: A-151
Keywords: Hepatocellular carcinoma, Liver transplantation, Malignancy, Waiting lists
Session Information
Session Name: Poster Session A: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Liver transplantation has been approved for hepatocellular carcinoma (HCC), hilar cholangiocarcinoma (CCA) and metastatic neuroendocrine tumors (NET), with the aim to produce similar outcomes as non-tumor patients and as such MELD exception points are granted in an effort to create equality both in waiting list opportunities and outcomes post-transplant. This study looks to determine if this equality exists within these three tumor types with regards to waiting list mortality.
*Methods: The Scientific Registry of Transplant Recipients database was analyzed for all patients listed for liver transplantation from 2002 to 2018, specifically looking at HCC, CCA and NET patients. The primary outcome was survival on the waiting list. Survival estimates were calculated from patients who dropped off the waiting list due to death or being too sick to transplant.
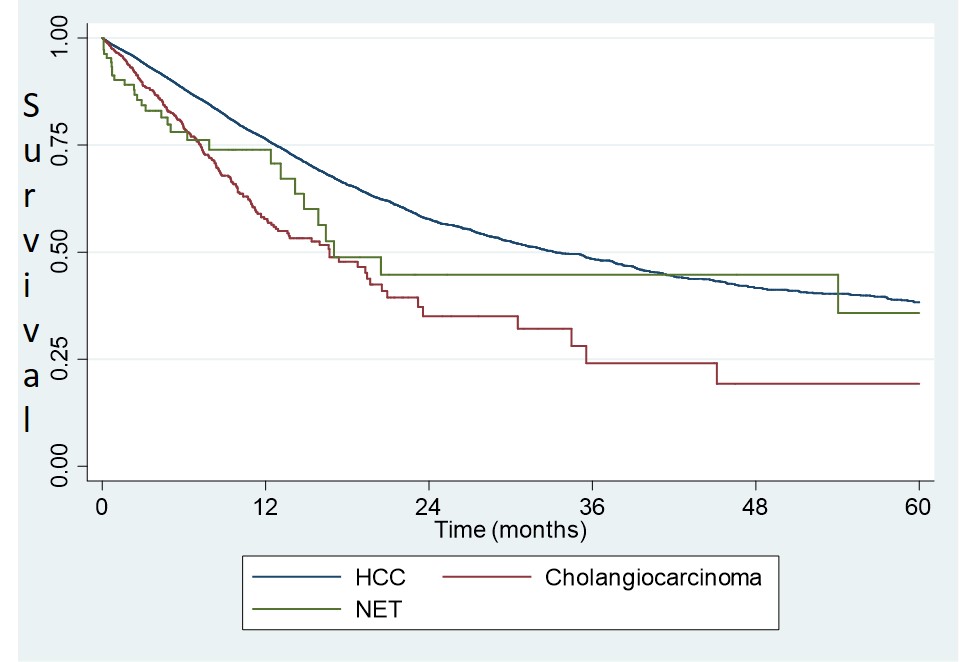
*Results: A total of 30858 patients were analyzed. There were 29856 HCC patients, 891 CCA and 111 NET patients. Unadjusted overall wait list drop-off at five years was significantly higher in the CCA (27.4%) and NET (27.0%) groups compared to the HCC group (17.8%) (p<0.001). Overall 5 year survival was 19%, 35% and 38% in the CCA, NET and HCC groups respectively (figure 1). Over time the HCC group had a stable drop in survival, whereas the CCA group had the largest drop off within the first year (58%) of listing. The NET group had its largest drop off in between the first (74%) and second (45%) years of listing.
*Conclusions: Patients with HCC are less likely to drop off the waitlist compared to CCA and NET. HCC patient survival steadily dropped annually, and this could either be due to tumor progression or background liver disease. Survival in the NET group was similar at 2 years and 5 years, with 29 of 30 (96.7%) reported deaths occurring in the first two years from disease that possibly had poor features, suggesting more indolent disease in survivors. CCA trended towards poorer outcomes at every time point and overall is known to be an aggressive disease. Some centers favor a cytoreductive approach for NET with surgical and radiological interventions and this is reasonable since most patients who survive two years without transplant have good overall survival, though alternatively one could define a NET subset who have bad disease, needing a liver transplant early to survive, and give them preference on the list. The CCA group overall seems disadvantaged, as without a transplant, their survival decreases rapidly each year and so perhaps an overall re-tooling of MELD exception points for CCA can be undertaken to produce more equality of waitlist survival comparable to the HCC and NET groups.
To cite this abstract in AMA style:
Menon VG, Chen Y, Chang DC, Yeh H. Waiting List Mortality of Liver Tumors [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/waiting-list-mortality-of-liver-tumors/. Accessed March 12, 2026.« Back to 2020 American Transplant Congress