Use of Public Health Service Increased Risk Kidneys in Pediatric Renal Transplant Recipients: Recipient Characteristics
1Children's Hospital of Philadelphia, Philadelphia
2University of Pennsylvania, Philadelphia.
Meeting: 2018 American Transplant Congress
Abstract number: B226
Keywords: Cadaveric organs, Graft acceptance, Kidney transplantation, Pediatric
Session Information
Session Name: Poster Session B: Kidney: Pediatrics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Purpose: The number of donors labeled as Public Health Service Increased Risk (IR) is rising. This designation identifies organs from donors at 'increased risk' of transmitting blood-borne infections yet with negative pre-donation serologies; it is not a marker of organ quality. Factors associated with utilization of IR kidneys in pediatric transplant recipients are unknown.
Methods: Retrospective study of all deceased donor isolated renal transplant recipients with pediatric priority (age 0-21 years) in the United States during the 'increased risk' period (6/30/04-12/31/16). Recipients receiving IR kidneys (cases) were compared to those who did not (controls). Separate eras were defined by changes in pediatric priority, donor risk guidelines, and the opioid epidemic.
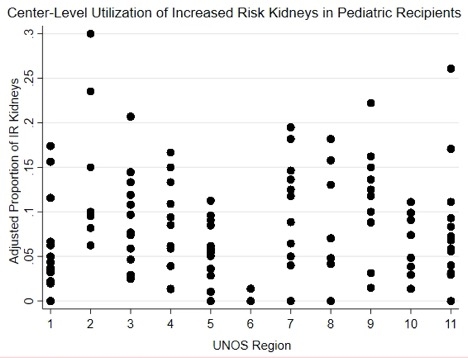
Results: 6938 pediatric patients received kidney transplants during the study period; 490 (7.1%) were IR kidneys. In multivariable mixed-effects models (center as random effect), recipient age, era, and blood type (type O) were significantly associated with receiving an IR kidney. Ethnicity/race, primary renal disease, maximum plasma reactive antibody, human leukocyte antigen mismatch, pre-transplant dialysis time, transplant waiting time and history of previous renal transplant were not associated with receiving an IR kidney. There was a significant interaction (p<0.001) between age and era, such that the relative odds of receiving an IR kidney based on age was not uniform across all eras. There appeared to be differences among centers within the same region in the proportion of kidney transplants from IR donors.
Conclusion: Risk factors for receiving an IR kidney in pediatric patients include recipient age, blood type, and era. There also appeared to be differences in the proportion of IR transplants by center within the same region. Further studies should investigate local and regional factors impacting centers' decisions to transplant or decline IR kidneys for pediatric recipients and the long-term outcomes of these decisions.
CITATION INFORMATION: Meyers M., Shults J., Laskin B., Porrett P., Levine M., Abt P., Amaral S., Goldberg D. Use of Public Health Service Increased Risk Kidneys in Pediatric Renal Transplant Recipients: Recipient Characteristics Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Meyers M, Shults J, Laskin B, Porrett P, Levine M, Abt P, Amaral S, Goldberg D. Use of Public Health Service Increased Risk Kidneys in Pediatric Renal Transplant Recipients: Recipient Characteristics [abstract]. https://atcmeetingabstracts.com/abstract/use-of-public-health-service-increased-risk-kidneys-in-pediatric-renal-transplant-recipients-recipient-characteristics/. Accessed June 30, 2025.« Back to 2018 American Transplant Congress