Ultrasound Targeted Microbubble Cavitation During Ex Vivo Normothermic Machine Perfusion Reduces Peribiliary Vascular Plexus Thrombi and Graft Injury in a DCD Liver Transplant Model
1Transplant Surgery, University of Pittsburgh, Pittsburgh, PA, 2Center for Ultrasound Molecular Imaging and Therapeutics, University of Pittsburgh, Pittsburgh, PA, 3Transplant Pathology, University of Pittsburgh, Pittsburgh, PA, 4Center for Biological Imaging, University of Pittsburgh, Pittsburgh, PA, 5Thomas E Starzl Transplant Inst, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 946
Keywords: Donors, non-heart-beating, Ischemia, Liver preservation, Ultrasonography
Topic: Basic Science » Basic Science » 15 - Machine Perfusion and Organ Rehabililtation - Basic
Session Information
Session Name: Machine Perfusion and Organ Rehabilitation - Basic
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Thrombus formation in the peribiliary vascular plexus (PBP) is a proposed mechanism for ischemic cholangiopathy (IC) after liver transplantation from donors after circulatory death (DCD). We hypothesized that DCD livers subjected to ultrasound (USG)-targeted microbubble (MB) cavitation while undergoing ex-vivo normothermic oxygenated machine perfusion (NMP) would clear PBP thrombi to flow, oxygenation, and function. This process of mechanical thrombolysis is termed sonothrombolysis (STL).
*Methods: In a rat DCD model with 30 minutes of warm ischemia time, livers received 4 hrs ex-vivo NMP. “Control” livers received NMP alone while “STL” livers received infusion of MB (perfluorocarbon-filled lipid spheres, 1-3 µm diam) in the hepatic artery (HA) for 15 min of each hour during the 4-hr NMP with USG to the liver parenchyma at 1.3 MHz and 1.6 mechanical index. Vascular flow and pressure measurements and perfusate and bile samples were taken throughout the 4-hr NMP. Tissue histology was assessed.
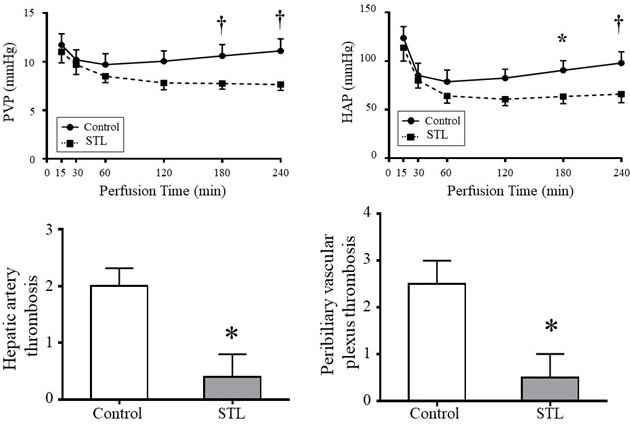
*Results: At a constant NMP flow rate, STL livers showed reduction in HA pressure as compared to Controls, consistent with a reduction in vascular resistance (p ˂0.01). During NMP, Controls showed a time-dependent increase in PV pressure, while STL livers showed gradual decline in PV pressure, becoming significant at 180 minutes (*: P ˂0.05 and †: P <0.01). Oxygen consumption by STL livers was higher vs Controls (p ˂0.05), suggesting better graft function. STL livers showed reduced ischemic injury, including lower perfusate ALT (p<0.001), higher biliary pH (p ˂0.05), lower biliary glucose (p˂0.05), and lower biliary LDH (p˂0.05). Bile duct histologic scoring showed less thrombi deposition in HA and PBP of STL livers compared to Controls (*p ˂0.05). Electron microscopy revealed that sinusoidal endothelium and biliary epithelial microvilli were better preserved in STL livers vs Controls.
*Conclusions: STL on a platform of NMP improved liver vascular flow, reduced HA and PBP clotting, and reduced hepatocyte and biliary injury in a rat DCD model. This method is proposed as an additive process to NMP to potentially reduce ischemic injury and IC in DCD liver transplants.
To cite this abstract in AMA style:
Nigmet Y, Hughes C, Chen X, Demetris A, Stolz D, Pacella J, Humar A, Villanueva F. Ultrasound Targeted Microbubble Cavitation During Ex Vivo Normothermic Machine Perfusion Reduces Peribiliary Vascular Plexus Thrombi and Graft Injury in a DCD Liver Transplant Model [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/ultrasound-targeted-microbubble-cavitation-during-ex-vivo-normothermic-machine-perfusion-reduces-peribiliary-vascular-plexus-thrombi-and-graft-injury-in-a-dcd-liver-transplant-model/. Accessed March 7, 2026.« Back to 2022 American Transplant Congress