Treatment of Late Antibody-Mediated Rejection: Observations from Clinical Practice.
1Nephrology, Medical School of Hannover, Hannover, Germany
2Pathology, Medical School of Hannover, Hannover, Germany.
Meeting: 2016 American Transplant Congress
Abstract number: C26
Keywords: Graft failure, Immunosuppression, Rejection
Session Information
Session Name: Poster Session C: Antibody Mediated Rejection: Session #1
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Antibody-mediated rejection (AMR) is a major cause of late renal allograft failure. The benefit of treatment of chronic ABMR is unknown. Currently there is no consensus for management of these pts.
We retrospectively evaluated the clinical management of pts with AMR in our department. Treatment decisions were made by the attending physician based on histology, antibody status, kidney function and other medical conditions. We assessed all pts who had a kidney transplant biopsy between 01/2009 and 12/2013. Of 2188 biopsies, n=424 were indication biopsies taken > 1 year post Tx in 280 pts. Of these, 120 biopsies were diagnosed with AMR by histology. Graft survival in pts with late AMR (n=71) was lower than in pts without histologic AMR (n=209) (p<0.0001) (Fig.1a). Of the pts with AMR, 39 were treated for AMR (plasmapheresis + IvIg +/- Rituximab), while 32 received no specific treatment (clinical decision). In 23% of pts treated for AMR, histology was suspicious but did not meet formal criteria for diagnosis of AMR. Of 39 pts with AMR treatment, only 21 had donor specific HLA-antibodies (DSA+); 11 were PRA+ but DSA-, and 6 had no HLA-antibodies. Graft survival in PRA+/DSA- pts was as poor as in DSA+ pts. Treatment of AMR had no effect on graft survival (Fig.1b). Pts who received treatment for AMR had more often combined chronic/active lesions (50% vs 32%, p=0.045) and less often only chronic features of AMR in the biopsy (11% vs 34%, p=0.006) than those without treatment. Other clinical characteristics were similar in pts with and without treatment: time post Tx 69±37 vs 59±38 months (p=0.16); creatinine 306±209 vs 322±232 [micro]mol/l (p=0.72); interstitial fibrosis 36±25% vs 30±28% (p=0.26) ; glomerulitis score (1.3±1,1 vs 1,4±1,2; p=0.66)), capillaritis (0.9±1.1 vs 0.8±1.0; p=0.71), transplant glomerulopathy (1.6±1.4 vs 1.6±1.3; p=0.96).
We observed considerable variation in clinical management of pts with late AMR. Treatment decisions are influenced by the clinical impression and in a significant number of cases do not apply established diagnostic thresholds. We could not demonstrate any beneficial effect of treatment of late AMR. 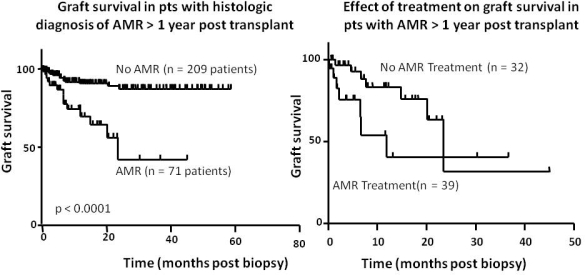
CITATION INFORMATION: Einecke G, Bräsen J, Schwarz A, Haller H, Njau F. Treatment of Late Antibody-Mediated Rejection: Observations from Clinical Practice. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Einecke G, Bräsen J, Schwarz A, Haller H, Njau F. Treatment of Late Antibody-Mediated Rejection: Observations from Clinical Practice. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/treatment-of-late-antibody-mediated-rejection-observations-from-clinical-practice/. Accessed March 3, 2026.« Back to 2016 American Transplant Congress
