Transitional B Cell T1/T2 Ratio Is a Prognostic Marker for Human Renal Allograft Deterioration.
1UPMC, Pittsburgh
2University of Leeds, Leeds, United Kingdom.
Meeting: 2016 American Transplant Congress
Abstract number: A176
Keywords: B cells, Graft survival, Idiopathic pulmonary fibrosis
Session Information
Session Name: Poster Session A: Kidney: Acute Cellular Rejection
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
Human transitional B cells (TrB) may play a significant role in auto and alloimmune disease. TrB express a high IL10:TNFα ratio and this fell with rejection. TrB are comprised of less mature T1 and more mature T2 cells. We characterized the cytokine expression of T1 vs. T2 cells (identified by differences in CD24&CD38 expression) and investigated the utility of T1/T2 ratio as a biomarker for allograft deterioration (graft loss or 50% decline in eGFR).
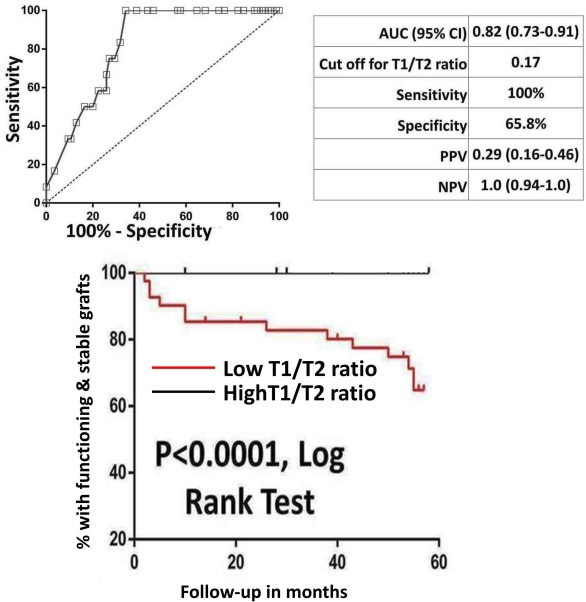
While both T1 and T2 cells expressed similar IL10, T1 cells expressed less TNFα and had a higher IL10:TNFα ratio. Thus T1 represent the B subset with the most anti-inflammatory profile. T1 cells were found to fall in rejection (resulting in lower T1/T2 ratio), contributing to low IL10:TNFα ratio. When analysed in 84 patients, T1/T2 ratio was a strong predictor of allograft deterioration over 5 years (ROC AUC 0.84, P<0.001) and was independently associated with allograft deterioration (per increase in the ratio by 1:HR 0.9, P=0.007). T1/T2 ratio was examined 2 years post Tx in a validation set of 97 stable patients derived from an RCT comparing alemtuzumab (n=51) or basiliximab induction (n=46). T1/T2 ratio was a strong predictor of outcome over the next 5 years (ROC AUC 0.82, P<0.001) and was independently associated with allograft deterioration (HR 0.88, P=0.02). Thus, the T1/T2 ratio can segregate clinically quiescent patients into two halves. Those with a high ratio will have entirely stable function, whereas in the group with a low ratio, ~35% had allograft deterioration over the ensuing five years (Fig-1). In both the test and validation sets, T1/T2 ratio was a much stronger predictor of graft deterioration than traditional markers like eGFR (test set, eGFR ROC AUC 0.76 vs. T1/T2 ratio 0.84; validation set, eGFR AUC 0.64 vs. T1/T2 0.82), or the detection of DSA (test set, DSA ROC AUC 0.68 vs. T1/T2 ratio 0.84; validation set, DSA AUC 0.66 vs. T1/T2 0.82).
To conclude, we demonstrate a distinct subset of TrB (T1) characterized by an anti-inflammatory cytokine profile. A decrease in T1:T2 ratio (due to selective loss of T1 cells) is a strong prognostic biomarker for subsequent renal allograft deterioration.
CITATION INFORMATION: Cherukuri A, Rothstein D, Baker R. Transitional B Cell T1/T2 Ratio Is a Prognostic Marker for Human Renal Allograft Deterioration. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Cherukuri A, Rothstein D, Baker R. Transitional B Cell T1/T2 Ratio Is a Prognostic Marker for Human Renal Allograft Deterioration. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/transitional-b-cell-t1t2-ratio-is-a-prognostic-marker-for-human-renal-allograft-deterioration/. Accessed February 15, 2026.« Back to 2016 American Transplant Congress
