Transitional B Cell Cytokines for the Early Prediction of Long-Term Renal Allograft Decline
1Starzl Transplantation Institute, UPMC, Pittsburgh, PA, 2UCL, London, London, United Kingdom
Meeting: 2020 American Transplant Congress
Abstract number: A-319
Keywords: Alloantibodies, B cells, Graft failure
Session Information
Session Name: Poster Session A: Biomarkers, Immune Assessment and Clinical Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Early prediction of allograft loss using potentially modifiable risk factors is vital for conceiving novel therapeutic interventions to improve outcomes.
*Methods: In this prospective, multicenter observational study designed to predict acute rejection in the 1st post-transplant year, we enrolled a total of 345 adult kidney transplant recipients and assessed several donor, recipient and clinical non-invasive variables at 3mos. We aimed to examine their association with a composite of overall graft loss and decline (defined as >30% loss in eGFR from baseline+ eGFR<30ml/min). IS utilized either thymo/Simulect induction followed by Tac+MMF. Based on the ability of the transitional B cell (TB) IL10/TNF expression ratio to predict rejection, we asked if the TB cytokine ratio in combination with other clinical variables measured at could predict allograft loss and decline over a 5year follow-up period. B cell cytokines were analyzed after a 24hr stimulation (CpG+CD40L) by flowcytometry.
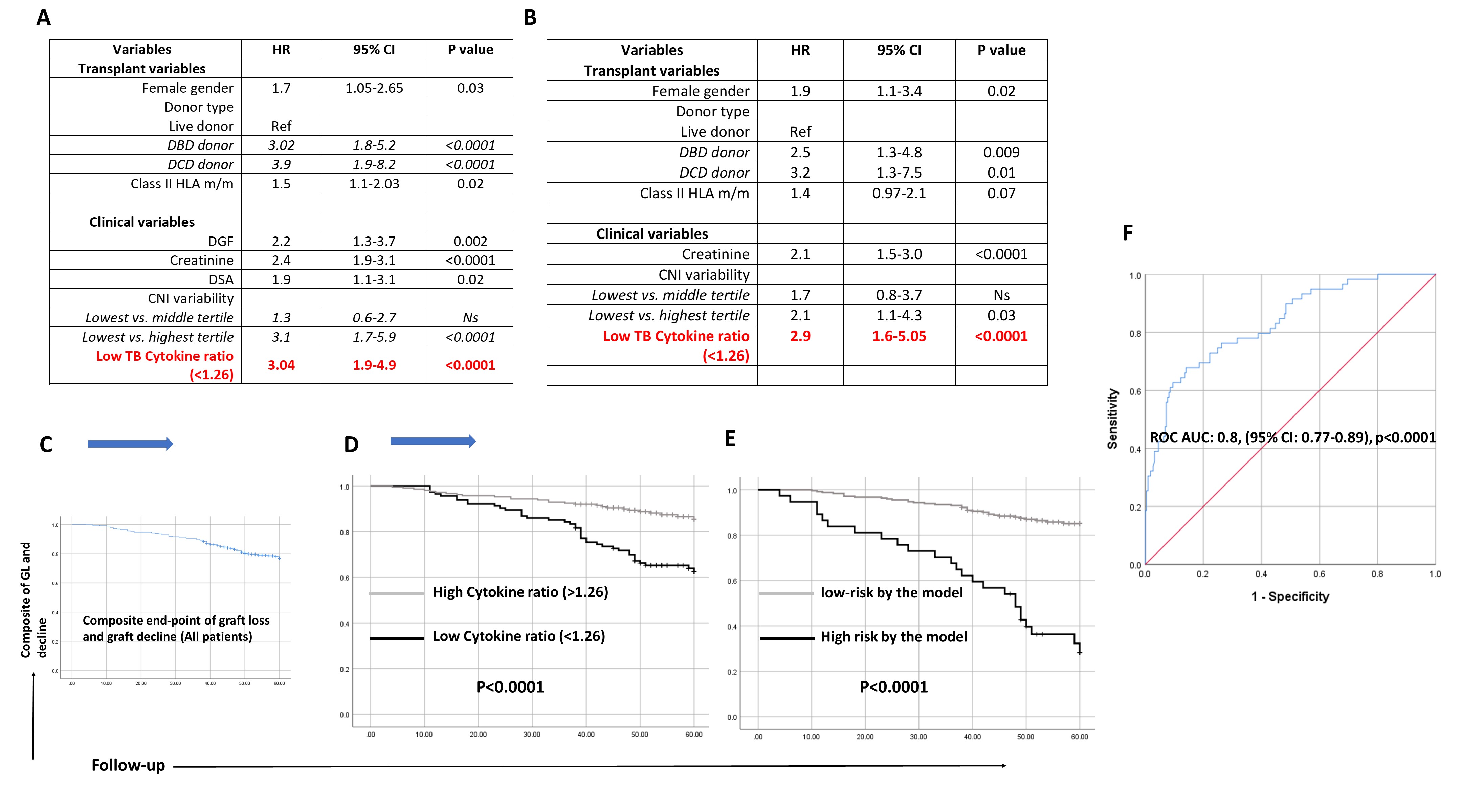
*Results: Of the factors examined, female recipient gender, donor type, Class II HLA mismatch, DGF, DSA detection, seCr at 3mos, intra-personal variability of CNI levels (CNI-IPV), and the TB IL10/TNF ratio measured at 3mos were significantly associated with the graft loss/decline at 5yrs (Fig1A). As shown in Fig 1B, a low T1B cytokine ratio was independently associated with graft loss/decline in a multivariate Cox regression model. In fact, the cytokine ratio itself, was able to risk stratify the patient cohort (with a 22% graft loss/decline) into those within high risk or low risk sub-groups with significantly different rate of allograft decline/loss (high cytokine ratio: 14% vs. low cytokine ratio: 37.5% graft loss/decline) (Fig 1C and 1D). Finally, addition of other significant factors (recipient gender, donor type, Se Cr at 3mos, CNI-IPV & DR HLA mismatch) to the TB cytokines improved risk stratification (high risk: 72% graft loss/decline vs. low risk: 15%) further (Fig 1E). This translated to a ROC AUC 0.83, p<0.0001 (optimal sensitivity of 98% with specificity of 70%), suggesting good predictive ability (Fig 1F).
*Conclusions: Thus, early examination of TB cytokines at 3mos, in addition to routinely measured and easily available clinical factors could predict allograft decline at a very early time point after transplantation. These results need to be validated in larger, prospective patient cohorts.
To cite this abstract in AMA style:
Cherukuri A, Salama A, Sharma A, Mehta R, Hariharan S, Rothstein D. Transitional B Cell Cytokines for the Early Prediction of Long-Term Renal Allograft Decline [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/transitional-b-cell-cytokines-for-the-early-prediction-of-long-term-renal-allograft-decline/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress