Transgenic Beta-cell Cxcl12 Expression and Stem Cell Mobilization Synergize to Suppress Type 1 Diabetes
Vaccine & Immunotherapy Center, Massachusetts General Hospital and Harvard Medical School, Boston, MA
Meeting: 2021 American Transplant Congress
Abstract number: 527
Keywords: Autoimmunity, Bone marrow, Hyperglycemia, Tolerance
Topic: Basic Science » Cellular Therapies, Tissue Engineering/Regenerative Medicine
Session Information
Session Name: Cellular Therapies, Tissue Engineering/Regenerative Medicine
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
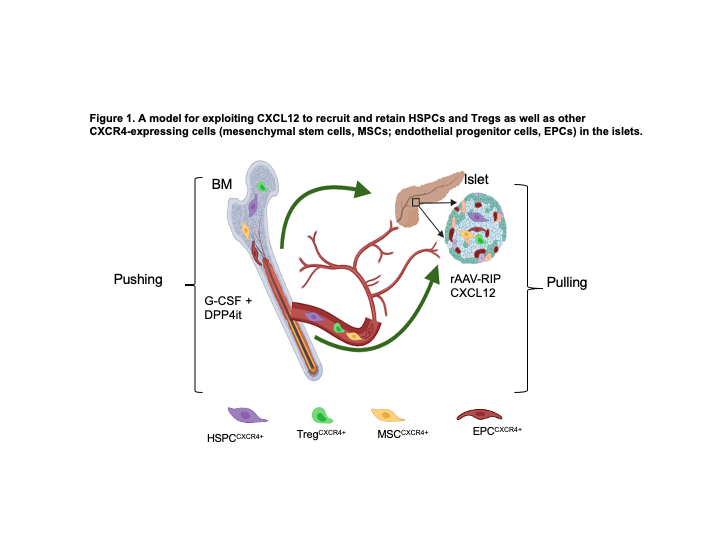
*Purpose: Hematopoietic stem and progenitor cells (HSPCs) and regulatory T cells (Tregs) highly express CXCR4, the receptor for the CXCL12 chemokine. This keeps them predominantly anchored to the bone marrow (BM) where CXCL12 is constitutively expressed at high levels. HSPCs and Tregs possess superior immunoregulatory properties and infusion of autologous HSPCs and Tregs is intensively investigated as a treatment for type 1 diabetes (T1D), which results from autoimmune-mediated destruction of insulin-producing β cells. β cells also express CXCR4 and CXCL12 exerts growth and pro-survival effects on them and can repel autoreactive T cells from islets. We hypothesized that CXCL12 could be exploited to recruit and retain endogenous HSPCs and Tregs in the islets to ameliorate autoimmune destruction of β cells and support β-cell survival and growth (Figure 1).
*Methods: We evaluated this hypothesis in NOD mice that spontaneously develop autoimmune diabetes.
*Results: CXCL12 levels were 3-fold higher in the BM of autoimmune diabetic NOD mice compared with age matched non-diabetic C57BL/6 mice. In reverse, the activity of DPP4, an exopeptidase that cleaves and inactivates the chemotactic effects of CXCL12, was ~2-fold lower in the BM of these NOD mice compared with their age matched C57BL/6 mice. This dysregulation of CXCL12 could contribute to polarized BM retention and impaired peripheral mobilization of HSPCs and Tregs in T1D. We showed that ectopic β-cell-specific expression of CXCL12 transgene under the control of the rat insulin promoter using a recombinant adeno-associated virus vector (p<0.05) and peripheral mobilization of HSPCs using granulocyte-colony stimulating factor plus DPP4 inhibitor treatment (p<0.06) delay autoimmune diabetes onset in NOD mice. Intriguingly, ectopic β-cell expression of CXCL12 synergized with peripheral mobilization to suppress autoimmune diabetes compared with either treatment alone (p<0.02; n≥10 per group). This synergy was characterized by increased numbers of circulating HSPCs, reduced insulitis, improved glucose tolerance and enhanced β-cell mass.
*Conclusions: Our findings demonstrate proof-of-concept of a novel “pushing” and “pulling” approach for T1D treatment.
To cite this abstract in AMA style:
Alagpulinsa DA, Jajoo A, II MHChapin, Poznansky MC. Transgenic Beta-cell Cxcl12 Expression and Stem Cell Mobilization Synergize to Suppress Type 1 Diabetes [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/transgenic-beta-cell-cxcl12-expression-and-stem-cell-mobilization-synergize-to-suppress-type-1-diabetes/. Accessed March 7, 2026.« Back to 2021 American Transplant Congress