Transcatheter Relief of Symptomatic Hepatic Venous Outflow Obstruction Following Pediatric Liver Transplantation.
Cincinnati Children's Hospital, Cincinnati, OH
Meeting: 2017 American Transplant Congress
Abstract number: B277
Keywords: Graft function, Liver grafts, Liver transplantation, Vascular disease
Session Information
Session Name: Poster Session B: Pediatric Liver Transplant - Clinical
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Background: Technical-variant allograft (TVA) pediatric liver transplantation (LT) is associated with vascular complications. Early recognition and treatment of hepatic venous outflow obstruction (HVOO) may be critical to optimizing outcomes.
Methods: Single-center case series of pediatric TVA recipients with HVOO and clinical sequelae from 12/2015-12/2016. All patients underwent cardiac catheterization (cath). Hemodynamic and angiographic assessment was followed by percutaneous intervention.
Results: 3 patients underwent transcatheter relief of HVOO at a median age of 14.3 yrs (range 1.8-16.1) and interval from LT of 244 days (88-433). Indications for LT: biliary atresia, cystic fibrosis and hepatic adenomatosis with neoplasms; indications for intervention: refractory ascites (n=2) and persistently elevated serum transaminases (n=1). In 2 patients, balloon venoplasty performed in interventional radiology did not provide clinical benefit. In all cases, cath demonstrated complex venous obstruction involving both the peri-hepatic inferior vena cava (IVC) and HV with a median gradient of 4 mmHg (4-8) and non-phasic pressure waveform in the HV.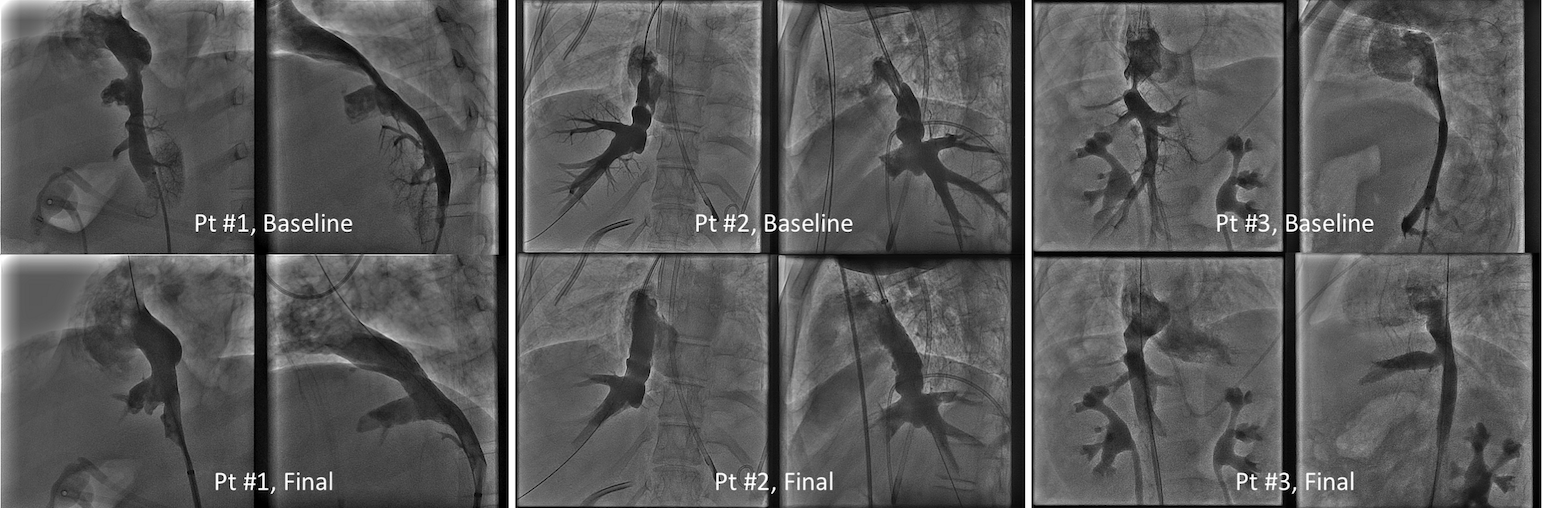 Compliant balloon venoplasty differentiated between dynamic (n=1) and fibrotic (n=2) stenosis. Dynamic obstruction was treated with balloon-expandable stent placement in the stenotic IVC, across the HV egress, with post-implant stent modification to create an unobstructed HV outflow. Fibrotic obstruction was treated with serial high pressure venoplasty of the HV and IVC with (n=1) or without (n=1) stent placement. Complete relief of HVOO was demonstrated in all cases with median residual gradient of 0 mmHg (0-1 mmHg), restoration of normal phasic HV waveform, and clinical resolution of ascites or decrease in serum transaminases. At a median follow-up of 2.3 months (0.8-11.4), all patients remain free of recurrent HVOO and associated clinical symptoms.
Compliant balloon venoplasty differentiated between dynamic (n=1) and fibrotic (n=2) stenosis. Dynamic obstruction was treated with balloon-expandable stent placement in the stenotic IVC, across the HV egress, with post-implant stent modification to create an unobstructed HV outflow. Fibrotic obstruction was treated with serial high pressure venoplasty of the HV and IVC with (n=1) or without (n=1) stent placement. Complete relief of HVOO was demonstrated in all cases with median residual gradient of 0 mmHg (0-1 mmHg), restoration of normal phasic HV waveform, and clinical resolution of ascites or decrease in serum transaminases. At a median follow-up of 2.3 months (0.8-11.4), all patients remain free of recurrent HVOO and associated clinical symptoms.
Conclusion: HVOO is a clinically-relevant complication of TVA pediatric LT. Lesion identification and definitive transcatheter therapy can relieve venous obstruction and related clinical symptoms.
CITATION INFORMATION: Goldstein B, Tiao G, Alonso M, Johnson N, Heubi J, Averin K, Bucuvalas J. Transcatheter Relief of Symptomatic Hepatic Venous Outflow Obstruction Following Pediatric Liver Transplantation. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Goldstein B, Tiao G, Alonso M, Johnson N, Heubi J, Averin K, Bucuvalas J. Transcatheter Relief of Symptomatic Hepatic Venous Outflow Obstruction Following Pediatric Liver Transplantation. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/transcatheter-relief-of-symptomatic-hepatic-venous-outflow-obstruction-following-pediatric-liver-transplantation/. Accessed March 6, 2026.« Back to 2017 American Transplant Congress
