Timing of Hypotension Post Kidney Transplant Impacts the Risk of Subsequent Delayed Graft Function
1Dalhousie University, Halifax, NS, Canada, 2Nova Scotia Health Authority, Halifax, NS, Canada
Meeting: 2022 American Transplant Congress
Abstract number: 843
Keywords: Graft function, Ischemia, Kidney, Surgical complications
Topic: Clinical Science » Kidney » 47 - Kidney Complications: Immune Mediated Late Graft Failure
Session Information
Session Name: Kidney Complications: Immune Mediated Late Graft Failure
Session Type: Poster Abstract
Date: Saturday, June 4, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-7:00pm
Presentation Time: 5:30pm-7:00pm
Location: Hynes Halls C & D
*Purpose: Hypotension is common post-kidney transplant and is associated with delayed graft function (DGF; a need for dialysis in the first week post-transplant) and prolonged hospitalization. Whether the timing of a hypotensive episode (ie. intra-operative, in the post-anaesthetic care unit (PACU), or when the patient returns to the floor after the PACU (on post-op day (POD) 0-7) might influence short term graft outcomes is unknown.
*Methods: We conducted a retrospective study of all adults patients undergoing kidney transplant in Atlantic Canada from 2006-2019. We identified patients who developed hypotension (defined as a systolic blood pressure <80 mmHg) over the first 7 days post-transplant, and categorized patients as experiencing hypotension i. in the operating room, ii. in the PACU, iii. on the floor (POD 0-7) or iv. no hypotension. We used multivariable logistic regression to determine the adjusted risk of DGF associated with a period of hypotension occurring at each of the three time periods, relative to those without hypotension. In a secondary analysis, we examined the outcome of prolonged length of stay (LOS) (greater than the median LOS for the entire cohort).
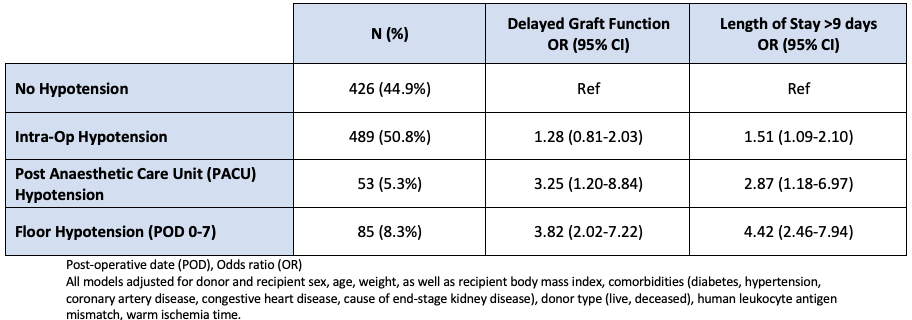
*Results: 1033 patients were included in the study; 170 (16.5%) developed DGF. In the first week post-op, hypotension occurred in 55.1% patients; 50.8% in the OR, 5.3% in the PACU, and 8.3% on the floor. Intra-op hypotension was not associated with DGF (OR 1.28, 95% CI 0.81-2.03), however hypotension in the PACU and on the floor were both significantly associated with DGF (OR 3.25, 95% CI 1.20-8.84 in PACU and OR 3.82, 95% CI 2.02-7.22 on the floor, respectively), Table 1. Amongst all patients, median LOS at the time of transplant was 9 days (Q1 7, Q3 13), and median LOS in those with hypotension at any point was 14 days (Q1 9, Q3 22). The risk of a prolonged LOS was significantly increased the later a hypotensive episode occurred (OR for a LOS >9 days was 1.51, 95% CI 1.09-2.10 for intra-op hypotension, OR 2.87, 95% CI 1.18-6.97 for PACU hypotension, and OR 4.42, 95% CI 2.46-7.94 for hypotension on the floor, relative to those without a hypotensive episode), Table 1.
*Conclusions: The timing of hypotensive episodes has a variable impact on the risk of both DGF and prolonged hospital LOS at the time of kidney transplant; the risk is highest in those with late hypotension (on the floor POD 0-7), followed by PACU, with intra-operative hypotension lowest risk. This supports a need for aggressive post-op blood pressure management that is not uniform at all time points post-transplant, and is an area for future study.
To cite this abstract in AMA style:
Morrison SA, Thanamayooran A, Tennankore K, Vinson AJ. Timing of Hypotension Post Kidney Transplant Impacts the Risk of Subsequent Delayed Graft Function [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/timing-of-hypotension-post-kidney-transplant-impacts-the-risk-of-subsequent-delayed-graft-function/. Accessed March 11, 2026.« Back to 2022 American Transplant Congress