Thrombolytic Therapy During Ex-Vivo Normothermic Machine Perfusion of Human Livers Reduces Peribiliary Vascular Plexus Injury
1Surgery, Beth Israel Deaconess Medical Center, Boston, MA, 2Massachusetts General Hospital, Boston, MA
Meeting: 2021 American Transplant Congress
Abstract number: 600
Keywords: Bile duct, Liver grafts, Machine preservation, Split-liver transplantation
Topic: Basic Science » Ischemia Reperfusion & Organ Rehabilitation
Session Information
Session Name: Ischemia Reperfusion & Organ Rehabilitation
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: A major limitation in expanding the use of DCD livers in transplantation are the higher rates of graft failure secondary to ischemic cholangiopathy. Warm ischemia causes thrombosis and injury to the peribiliary vascular plexus (PVP), which is supplied by branches of the hepatic artery, causing higher rates of biliary complications in DCD allografts. We aimed to recondition discarded DCD livers with tissue plasminogen activator (tPA) while on normothermic machine perfusion (NMP) to improve PVP blood flow and reduce biliary injury.
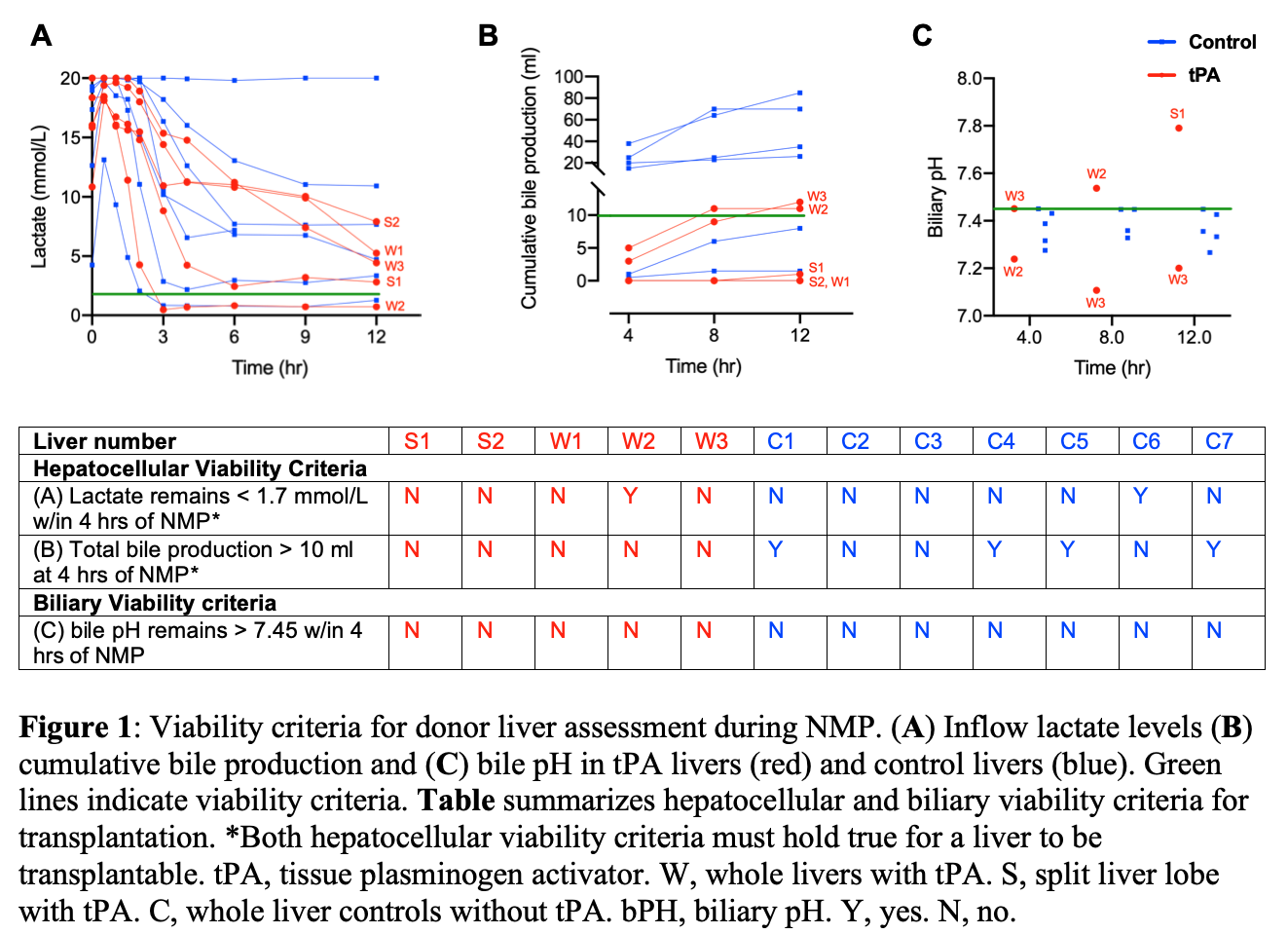
*Methods: Five discarded DCD human livers underwent 12 hours of NMP. Plasminogen was circulated in the base perfusate prior to initiation of perfusion and 1 mg/kg of tPA was administered through the hepatic artery at T=0.5 hours. Two livers were split prior to perfusion (S1, S2), with tPA administered in one lobe, while the other served as a control. The remaining three whole livers (W1-W3) were compared to seven DCD control liver perfusions (C1-C7) with similar hepatocellular and biliary viability criteria (fig 1). D-dimer levels were measured at T=1 hour to verify efficacy of tPA. Lactate, total bile production, bile pH, and difference in biliary injury scores before and after perfusion were compared between tPA and non-tPA groups using two-tailed t-tests.
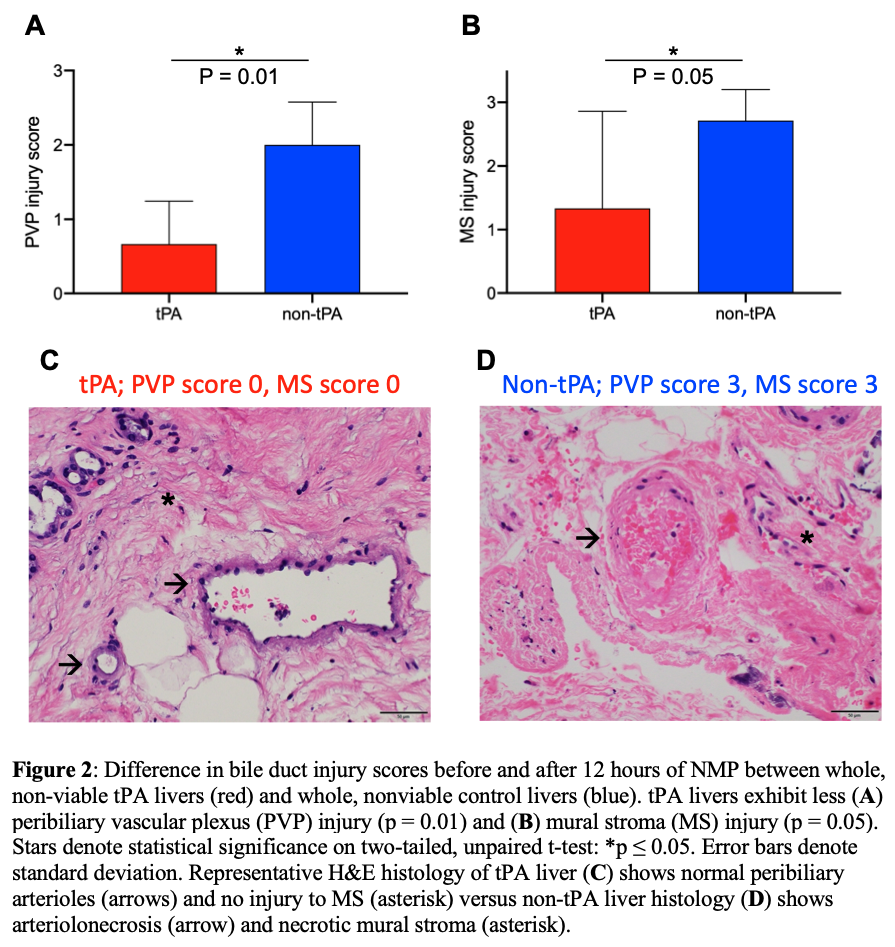
*Results: Average weight-adjusted D-dimer levels were higher in tPA livers in the split (p=0.002) and whole-liver model (p=0.02), verifying drug function. There were no differences in perfusion hepatic artery resistance, portal vein resistance, and arterial lactate between tPA livers and non-tPA livers in both the split and whole-liver model. However, when comparing biliary injury between hepatocellular and biliary non-viable whole livers, tPA livers had significantly lower PVP injury scores (0.67 vs. 2.0, p=0.01) and mural stroma (MS) injury scores (1.3 vs. 2.7, p=0.05) (fig 2).
*Conclusions: This study demonstrates that administration of tPA into DCD livers during NMP can reduce PVP and MS injury. Further studies are necessary to assess the effect of tPA administration on long term biliary complications.
To cite this abstract in AMA style:
Haque O, Raigani S, Rosales I, Carroll C, Coe TM, Baptista S, Yeh H, Uygun K, Markmann JF. Thrombolytic Therapy During Ex-Vivo Normothermic Machine Perfusion of Human Livers Reduces Peribiliary Vascular Plexus Injury [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/thrombolytic-therapy-during-ex-vivo-normothermic-machine-perfusion-of-human-livers-reduces-peribiliary-vascular-plexus-injury/. Accessed February 24, 2026.« Back to 2021 American Transplant Congress