The Predictive Factors of Survival in Re-listed Patients Who Received Initial Liver Transplants Using Donation After Circulatory Death Grafts
Cleveland Clinic, Cleveland, OH
Meeting: 2021 American Transplant Congress
Abstract number: 336
Keywords: Graft failure, Liver transplantation, Retransplantation, Survival
Topic: Clinical Science » Liver » Liver: Retransplantation and Other Complications
Session Information
Session Name: Post Liver Transplant Management and Complications
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 8, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:40pm-4:45pm
Presentation Time: 4:40pm-4:45pm
Location: Virtual
*Purpose: The inherent risk of livers from donors after circulatory death (DCD) is well known such as primary non-function (PNF) and increased rates of biliary complications. Due to the high graft dysfunction rate in a relatively early phase after the initial liver transplant (LT), many patients who received DCD organ needs re-transplant and were re-listed. However, the clinical characteristics and prognostic factors of those re-listed patients have not been fully elucidated.
*Methods: Adult patients who received DCD LT between 2002 and 2019 were identified from the UNOS database. Predictors of drop out due to too sick/death in re-listed patients were examined using Fine-Gray model. Predictors of overall survival (OS) after re-LT were examined using Cox regression model.
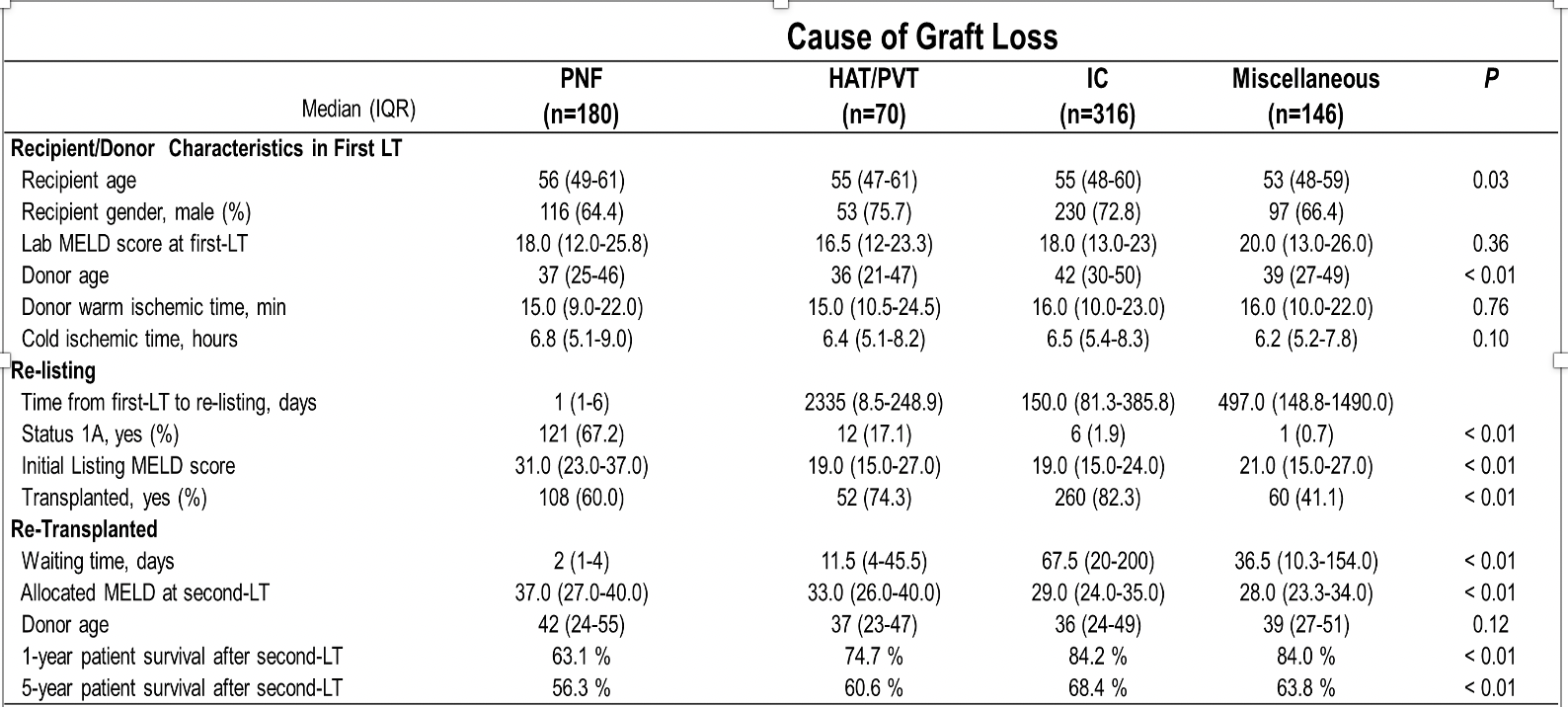
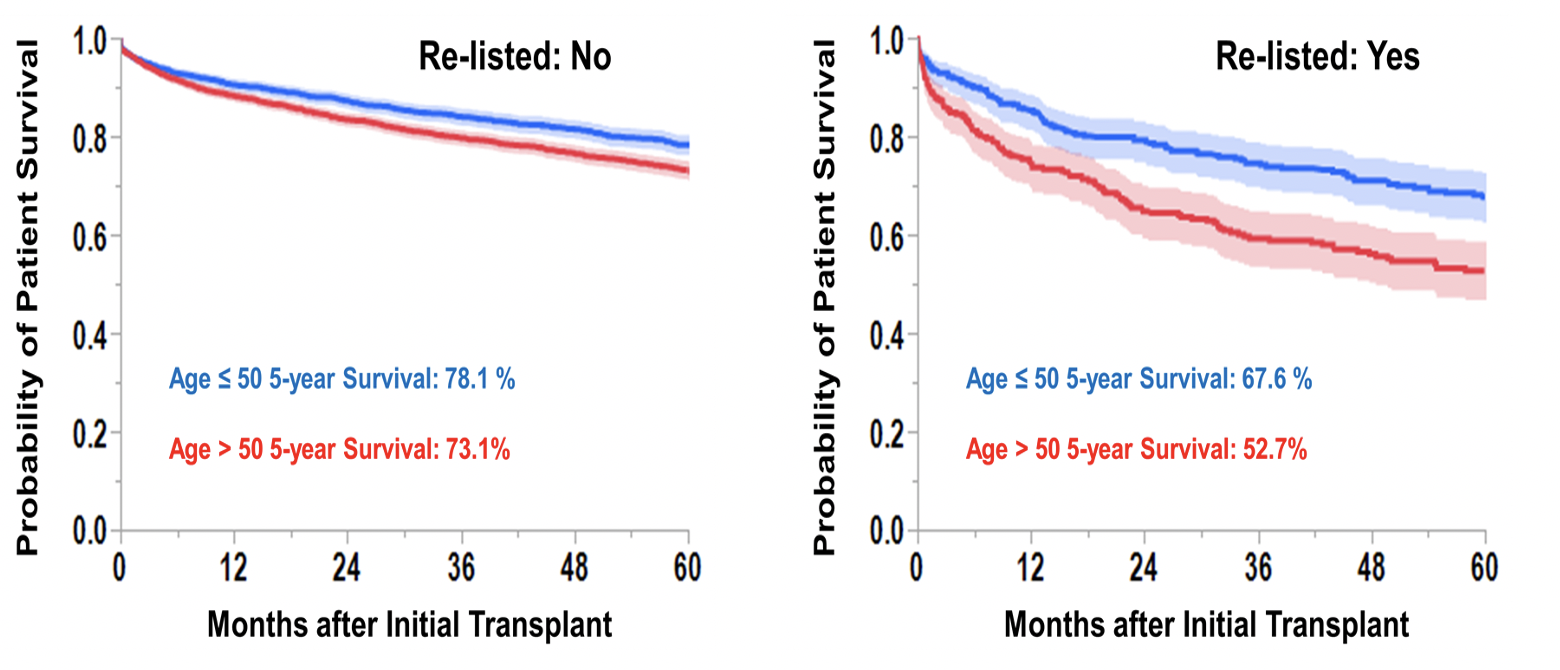
*Results: Among 5734 patients, 1332 patients died without re-listing (23.2%) and 712 patients were re-listed after initial LT (12.4%). Among 711 re-listed patients, 480 patients received second LT (8.4%) and 128 patients were removed from list because of too sick/death (2.2%). Among 480 re-LT patients, 187 patients (39.0%) died after re-LT. The median days between first LT and re-listing was 99 days (IQR: 12-331). The distribution of initial graft lost causes/percentage of re-LT patients/median waiting time form re-listing are summarized (Table). In re-listed patients, older recipient (> 50) and graft loss caused by primary non-function or HAT/PVT were predictors of dropout. In re-LT patients, younger recipient (≤50) at first-LT, male, lower MELD at time of second-LT, and younger donor age were favorable factors of patient survival after LT. The OS from first-LT was compared according to recipient age in patients who were re-listed and not re-listed. The 5-years survival rate in younger patients was 5.0% better in patient without re-listing, which was much higher in re-listed patients (14.9%) (Figure).
*Conclusions: Nearly 10% of DCD LT patients received re-LT mainly due to complications related to DCD organs. Younger recipient age is an important factor to survive in case patients need re-listing after LT using DCD organ.
To cite this abstract in AMA style:
Fouda Y, Moro A, Mcvey J, Firl D, Fujiki M, Teresa D, Aucejo F, Quintini C, Kwon CH, Hashimoto K, Eghtesad B, Menon KNarayanan, Miller C, Sasaki K. The Predictive Factors of Survival in Re-listed Patients Who Received Initial Liver Transplants Using Donation After Circulatory Death Grafts [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/the-predictive-factors-of-survival-in-re-listed-patients-who-received-initial-liver-transplants-using-donation-after-circulatory-death-grafts/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress