The Losing Trifecta: Age ≥70, Deceased Donor Transplant, and Delayed Graft Function
Columbia University, New York.
Meeting: 2015 American Transplant Congress
Abstract number: 442
Keywords: Age factors, Kidney transplantation, Mortality
Session Information
Session Name: Concurrent Session: Kidney - Delayed Graft Function and Older Age
Session Type: Concurrent Session
Date: Tuesday, May 5, 2015
Session Time: 4:00pm-5:30pm
 Presentation Time: 4:24pm-4:36pm
Presentation Time: 4:24pm-4:36pm
Location: Room 115-AB
INTRO: Patients ≥70 are the fastest growing part of the ESRD population. Although historically patients ≥70 have had acceptable renal transplant outcomes, in our own program, age ≥70 was one of the strongest risk factors for dying within one year of renal transplantation.
METHODS: We reviewed each elderly recipient's chart collecting pretransplant characteristics and comorbidities at time of evaluation to calculate the Charlson Comorbidity Score, and the 5 year mortality risk score developed by van Walraven* which includes comorbidities as well as wait-list and transplant specific variables. These individual factors were compared using univariate analysis to predict the risk of early mortality.
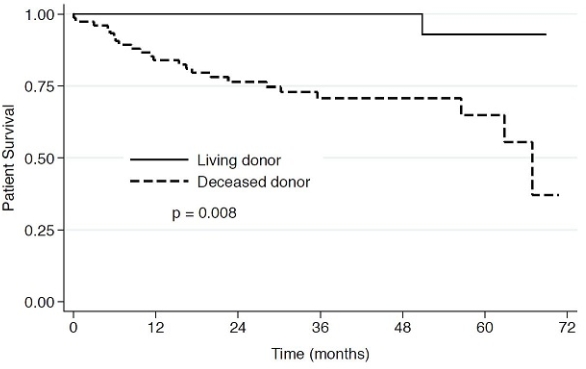
RESULTS: Between 2009-2013, we performed 1221 renal txp, of whom 110 were ≥70. Our elderly cohort had a median age of 71.5 (IQR:69.8-73.8) at listing and 73(IQR:71.1-75.3) at time of txp. They were mostly male (72.7%) and recipients of DDRTx (70.9%). After median follow up of 34.8 (18.5 -55) months, 8.2% experienced allograft failure and 21.8% died with functioning grafts. 14 of these 24 patients died in the first year. DGF was associated with higher rates of graft failure (58.1 vs 77.6%, p=0.035), as was rehospitalization [57.1% vs 87.3% (p=0.001)]. The Charlson Comorbidity Score and 5 year mortality prediction minimally correlated with survival (area under ROC curve∼ 0.7). The strongest predictor of mortality was receiving a DDRTx (OR=12) a risk which increased after adjusting for DGF (OR 16, CI= 1.96-133.4). Patients who died during follow up had significantly longer dialysis duration pretransplant (28.5±21.3 vs 47.1±35.5 months, p=0.005), an increase in risk of 2% for each month on dialysis, and were more likely to have been rehospitalized (87.5 vs 48.8%, p=0.001) despite being of similar age (73.6±3 vs 73.9±3.3, p=0.69).
CONCLUSION: Although overall outcomes with elderly transplant recipients are acceptable, careful donor and recipient selection cannot be overemphasized. These patients have a particular mortality benefit receiving a living donor versus deceased donor transplant.
* van Walraven C. et al. CMAJ 2010, 182(7) 666
To cite this abstract in AMA style:
Crew R, Fernandez H, Mohan S, Dube G, Ratner L, Sandoval R, Patel S. The Losing Trifecta: Age ≥70, Deceased Donor Transplant, and Delayed Graft Function [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/the-losing-trifecta-age-70-deceased-donor-transplant-and-delayed-graft-function/. Accessed July 15, 2025.« Back to 2015 American Transplant Congress
