The Long Term Impact of Metabolic Syndrome on Post-Donation in Living Kidney Donors
C. Chen, T. Yu, Y. Chuang, S. Tsai, M. Wu
Division of Nephrology, Taichung Veterans General Hospital, Taichung, Taiwan
Meeting: 2020 American Transplant Congress
Abstract number: C-076
Keywords: Donation, Kidney transplantation, Metabolic disease, Renal dysfunction
Session Information
Session Name: Poster Session C: Kidney Living Donor: Long Term Outcomes
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The long waiting list for kidney transplant (KTx) in Taiwan, the willingness of transplant centers increase to accept complex donors, eg. metabolic syndrome (MS). The goal of this study was to determine the impact of metabolic syndrome on their renal outcome in these living kidney donors.
*Methods: Between January 2000 and December 2018, a total of 366 living kidney donors who underwent donor nephrectomy at our institution were enrolled. Metabolic syndrome was diagnosed in patients according to the National Cholesterol Education Program’s Adult Treatment Panel III, were compared in participants with or without metabolic syndrome. Using multivariate regression analysis, the goal was to identify which component of metabolic syndrome induces chronic histologic changes and delayed renal function recovery.
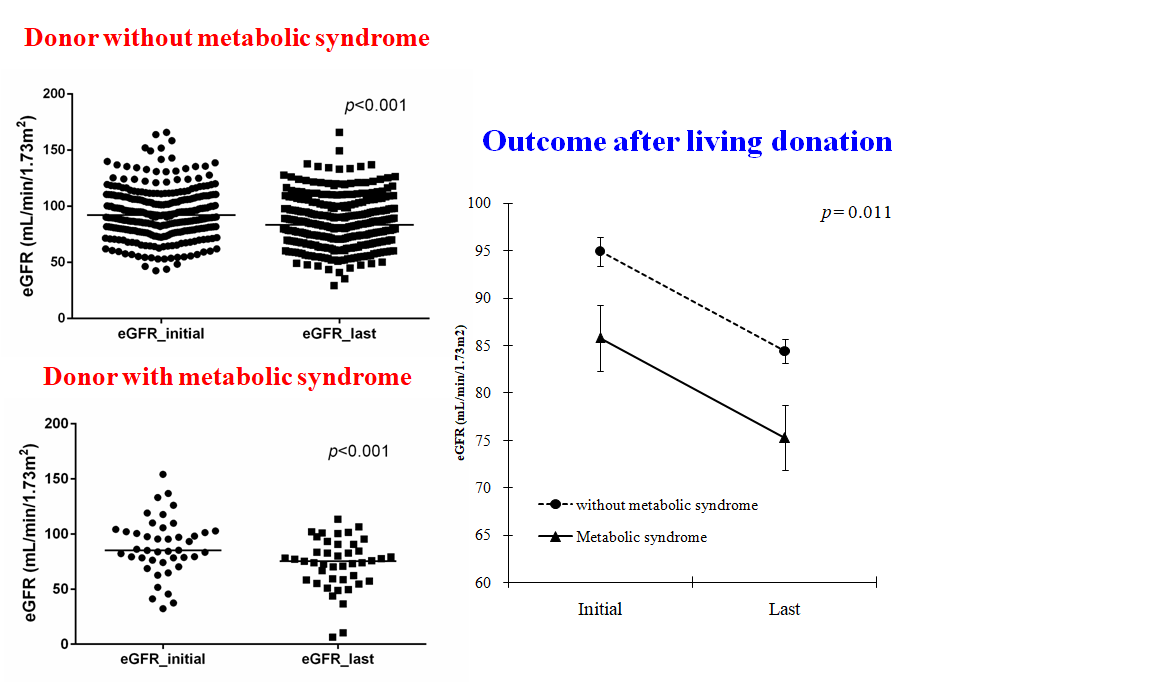
*Results: We identified 43 donors (11.7%) with metabolic syndrome. Donors with metabolic syndrome were older (51.4 ± 8.7 yrs vs 37.5 ± 10.1 years; P < .001) and more male gender (58.1% vs 34.4%; P = 0.004) than subjects without metabolic syndrome. Results of the multivariate regression analysis indicated that obesity, hyperglycemia, and hypertriglyceridemia were independently associated with their long-term outcome of renal function. Patients with metabolic syndrome were more likely to experience delayed renal function recovery. Though the initial eGFR was not significantly different between donors with metabolic syndrome (85.1 ± 7.4) to without ones ( 92.2 ± 8.3; P = 0.221), but the last eGFR was significantly different from donors with metabolic syndrome (75.2 ± 6.1) to without ones (83.3 ±7.1; P = 0.003).
*Conclusions: Although metabolic syndrome in living kidney donors is characterized by poor long-term renal function, the eGFR seemed to keep acceptable range in long-term follow-up. Obesity is the most important metabolic factor for predicting delayed renal function recovery in living kidney donors, providing an important clinical indicator of postoperative renal function in these patients.
To cite this abstract in AMA style:
Chen C, Yu T, Chuang Y, Tsai S, Wu M. The Long Term Impact of Metabolic Syndrome on Post-Donation in Living Kidney Donors [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-long-term-impact-of-metabolic-syndrome-on-post-donation-in-living-kidney-donors/. Accessed July 3, 2025.« Back to 2020 American Transplant Congress