The Impact of Donor Specific Alloantibodies on Long-Term Outcomes of Liver Re-Transplantation
1Department of Pathology and Lab Medicine, University of Western Ontario, London, ON, Canada
2Department of Surgery, University of Western Ontario, London, ON, Canada.
Meeting: 2018 American Transplant Congress
Abstract number: 240
Keywords: Alloantibodies, Graft survival, Liver transplantation, Retransplantation
Session Information
Session Name: Concurrent Session: Liver Retransplantation and Other Complications
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:42pm-2:54pm
Presentation Time: 2:42pm-2:54pm
Location: Room 6A
Despite reports that associate donor specific antibody (DSA) with rejection after liver transplantation, grafts are still allocated according to blood group (ABO) but not human leukocyte antigen (HLA) compatibility, possibly due to the absence of an easily discernible clinical association between adverse recipient outcome and DSA. Re-transplantation provides a test environment where the presence of preformed DSA is prevalent and its effect on outcome should be apparent.
Method: All patients undergoing a second liver transplantation with available pre-operative serum and donor cells were included with the exception of ABO incompatible or multiple organ transplants. Banked sera were tested for anti-HLA antibodies with Luminex-based solid phase assays. The threshold for positivity was median fluoresce intensity > 1000. Anti-HLA antibodies to the second donor (D2SA) were typed for HLA-A, B, C, DRB1, DRB3/4/5, DQA1/B1 and DPA1/B1.
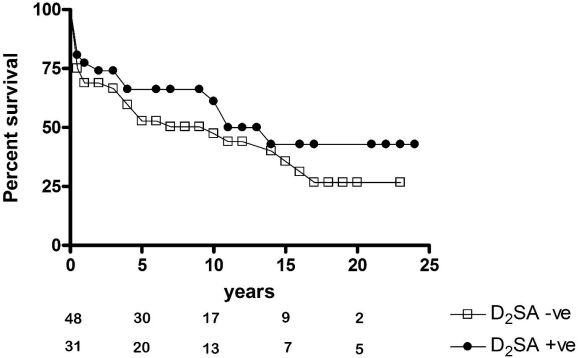
Results: Anti-HLA antibodies were identified before the second transplantation in 40 (51%) of the 79 patients that were included in the study. Primary and re-transplantation characteristics were similar in both groups except first graft survival which was significantly shorter in recipients who did not develop anti-HLA antibodies before the second transplantation. Preformed D2SA was identified in 31 (39%) patients, of whom 23 (74.2%) had D2SA directed to HLA-DQ. Median survival of the second graft was equivalent in the presence (D2SA+) or absence (D2SA-) of D2SA {11 (0 – 24) versus 10 (0 – 23) years respectively, p = 0.3}, as were the survival curves [figure 1]. Five (16%) of the D2SA+ patients compared to 4 (8%) of the D2SA- patients underwent a third liver transplantation (p = 0.3). To date, 11 (35%) of the D2SA+ patients compared to 27 (56%) of the D2SA- patients have died (p = 0.1). Subgroup analysis showed no effect of class, loci, strength of D2SA or of non-DSA anti-HLA antibodies on survival of the second liver transplant.
Conclusion: Presence of DSA was not found to be associated with inferior outcomes in this retrospective cohort study of liver re-transplantation.
CITATION INFORMATION: Xu Q., Skaro A., McAlister V. The Impact of Donor Specific Alloantibodies on Long-Term Outcomes of Liver Re-Transplantation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Xu Q, Skaro A, McAlister V. The Impact of Donor Specific Alloantibodies on Long-Term Outcomes of Liver Re-Transplantation [abstract]. https://atcmeetingabstracts.com/abstract/the-impact-of-donor-specific-alloantibodies-on-long-term-outcomes-of-liver-re-transplantation/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress