The Effect of Donor-Recipient Relationship on the Immunologic Outcome in Living Kidney Transplantation.
Nephrology, Charite Campus Mitte, Berlin, Germany.
Meeting: 2016 American Transplant Congress
Abstract number: A136
Keywords: Graft survival, Microchimerism, Rejection, Sensitization
Session Information
Session Name: Poster Session A: Kidney Donor Outcomes
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
Background. Presensitization and degree of HLA-matching influences immunologic outcome and kidney graft survival. Thus the donor-recipient relationship may influence incidence of immunologic events and outcome in living related kidney transplantation (KTx). The aim of the study was to analyze the long-term immunologic outcomes of living KTx depending on the donor-recipient relationship.
Materials and methods. This retrospective single center long-term observational study included kidney transplant recipients (KTR) between 2000 and 2014. KTR from living donors (178 pts) were categorized according to donor-recipient relationship: 65 KTx between siblings, 39 father-to-child (FtC) and 74 mother-to-child (MtC) donations. DSA analysis and allograft biopsies were performed for clinically suspected rejections. Data analysis included patient and graft survival, biopsy proven rejection episodes (T-cell mediated (TCMR) or antibody mediated (ABMR)) and development of de novo DSA. Outcome data were assessed over a period of maximal 14 years.
Results. There were no significant difference between the groups (siblings, FtC, MtC) with regards to HLA-mismatch, prior kidney transplantation, time on dialysis and cold ischemia time. Donor-recipient relationship had no significant influence on graft survival (Fig 1A). Among KTR with related donors FtC- and MtC-pares showed comparable incidences of TCMR, both significantly exceeding the rate in sibling-to-sibling pares (Fig 2B). The multivariant cox regression analysis adjusted for recipient age, donor age and HLA (A, B, DR)-mismatch identified both MtC and FtC donation as important independent risk factors for TCMR (HR 8.13, p<0.001 and HR 8.09, p=0.001, respectively). There was no significant difference between the groups in terms of ABMR (Fig. 1C) and development of de novo DSA (Fig. 1D) 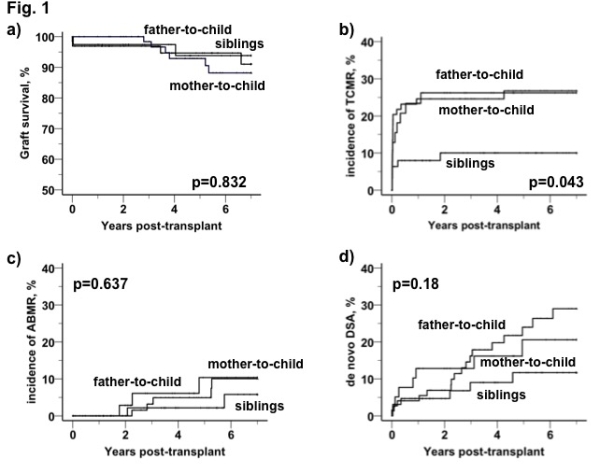 .
.
Conclusion. Our results point out parent-to-child kidney donation as an independent risk factor for TCMR.
CITATION INFORMATION: Khadzhynov D, Halleck F, Lehner L, Duerr M, Waiser J, Budde K, Staeck O. The Effect of Donor-Recipient Relationship on the Immunologic Outcome in Living Kidney Transplantation. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Khadzhynov D, Halleck F, Lehner L, Duerr M, Waiser J, Budde K, Staeck O. The Effect of Donor-Recipient Relationship on the Immunologic Outcome in Living Kidney Transplantation. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/the-effect-of-donor-recipient-relationship-on-the-immunologic-outcome-in-living-kidney-transplantation/. Accessed March 6, 2026.« Back to 2016 American Transplant Congress
