The Combined Effect of Acute Rejection and De Novo Donor-Specific Antibodies on Kidney Allograft Survival.
Division of Renal Diseases and Hypertension, University of Colorado, Aurora, CO.
Meeting: 2016 American Transplant Congress
Abstract number: D5
Keywords: Graft survival, HLA antibodies, Kidney transplantation, Rejection
Session Information
Session Name: Poster Session D: Antibody Mediated Rejection: Session #2
Session Type: Poster Session
Date: Tuesday, June 14, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
While dnDSA is associated with graft loss in multiple studies, the clinical context in which dnDSA develops and contributes to graft loss is less well defined. Acute rejection (AR) may lead to or result from the development of dnDSA and may be the primary determinant of graft outcomes. The purpose of this study was to delineate the relative timing and impact of AR and dnDSA on graft survival in what is to our knowledge the largest prospective DSA screening protocol analysis to date.
From 2007 to 2013, 598 consecutive kidney and kidney-pancreas recipients without pre-existing DSA were prospectively screened for dnDSA (MFI ≥ 500) using single-antigen beads at post-transplant months 1, 6, 12, yearly and when clinically indicated. Acute rejection was diagnosed by clinical suspicion and was biopsy-proven in 88% of cases. Graft survival was assessed by KM analysis and time-dependent Cox modeling with a median (IQR) follow-up time of 49 (31-69) months.
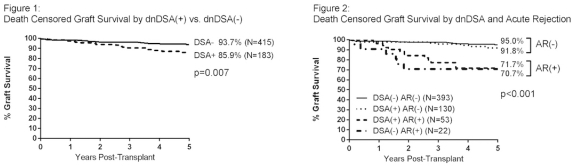
183 (30.6%) patients developed dnDSA (median onset 6.5 months). 5-year death-censored graft survival was lower in patients with dnDSA (Figure 1). AR was more common in dnDSA(+) vs. dnDSA(-) patients (29% vs. 5%, RR 5.5, 95% CI 3.4-8.7, p<0.001) and its timing relative to dnDSA detection did not affect graft outcomes. Patients with mixed class I and II dnDSA experienced more AR (RR 8.6, 95% CI 5.3-14.1, p<0.001) vs. those without dnDSA and had worse graft survival (dnDSA(-) 93.7%, class I 86.3%, class II 94.5%, mixed class 73.6%, p<0.001). When stratifying patients by AR and dnDSA status, 5-year graft survival was lower only in those patients with AR, regardless of dnDSA status (Figure 2). In a multivariable analysis that accounted for both dnDSA and AR, AR was strongly associated with graft loss (HR 8.7, 95% CI 4.4-17.4, p<0.001) while dnDSA alone failed to reach statistical significance.
In this large retrospective analysis of a prospective dnDSA screening protocol, both dnDSA and AR were associated with inferior intermediate term graft survival. Importantly, the deleterious impact of dnDSA on outcomes was only seen when combined with AR.
CITATION INFORMATION: Davis S, Gralla J, Wiseman A, Cooper J. The Combined Effect of Acute Rejection and De Novo Donor-Specific Antibodies on Kidney Allograft Survival. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Davis S, Gralla J, Wiseman A, Cooper J. The Combined Effect of Acute Rejection and De Novo Donor-Specific Antibodies on Kidney Allograft Survival. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/the-combined-effect-of-acute-rejection-and-de-novo-donor-specific-antibodies-on-kidney-allograft-survival/. Accessed February 21, 2026.« Back to 2016 American Transplant Congress
