The Changing Face of T Cell-Mediated Rejection
1Medical University of Warsaw, Warsaw, Poland, 2Alberta Transplant Applied Genomics Centre, Edmonton, AB, Canada
Meeting: 2019 American Transplant Congress
Abstract number: 424
Keywords: Biopsy, Gene expression, Kidney transplantation, Rejection
Session Information
Session Name: Concurrent Session: Kidney: Acute Cellular Rejection
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Ballroom C
*Purpose: We studied how the problem of TCMR in indication biopsies was changing with time by exploring features of 138 biopsies with molecular TCMR in 1745 indication biopsies in the INTERCOMEX study (ClinicalTrials.gov NCT01299168). We compared an earlier cohort (before 2012) to a more recent cohort to examine differences in the frequency, molecular picture, and outcomes after TCMR biopsies.
*Methods: Indication biopsies from 21 centers were processed by histology and microarrays. Biopsies with TCMR were selected based on their molecular MMDx class.
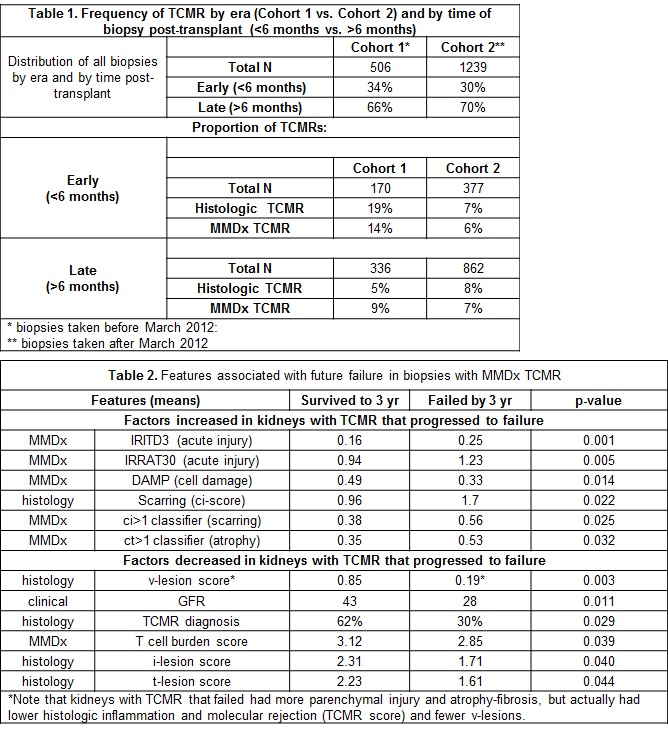
*Results: The proportion of early vs. late biopsies was similar in biopsies before 2012 (66%) vs. after 2012 (70%). TCMR in early biopsies was less frequent after 2012 (Table 1) but the frequency of TCMR in late biopsies was unchanged by histology (8%) or MMDx (7%). Kidney failure within 3 years occurred in 23/138 biopsies. Kidneys with TCMR that failed tended to be biopsied late (730 days post-transplant) and to have proteinuria at biopsy. Five were BK positive. Molecular TCMR was often missed by histology (and perhaps not treated). To determine why kidneys fail after TCMR, we compared 23 TCMR that failed within 3 years of biopsy to 26 with known graft survival >3 years post biopsy (Table 2). Among 67 clinical, histologic, and molecular variables, 11 were significant at the 0.05 level: molecular nephron injury (IRITD3, IRRAT30/AKI transcripts; damage-associated molecular patterns (DAMP)); atrophy-scarring (molecular cigt1 classifier and histologic ci>1), and GFR. Histologic v-, i- and t-scores were lower in failure group (failure was inversely related), presumably because of scarring. Molecular T cell burden was lower in kidneys that failed, although MMDx TCMR and rejection scores were similar (not shown). Determinants of failure after TCMR biopsies are predominantly recent molecular parenchymal injury and stage (atrophy-scarring), not molecular rejection and inflammation scores.
*Conclusions: Early TCMR is declining, but late TCMR remains a serious issue, often in kidneys with extensive parenchymal damage. Late TCMR is probably often due to non-adherence. Graft loss after late TCMR episodes is associated with severe nephron injury and parenchymal loss (atrophy-fibrosis), with low GFR at biopsy, but not with molecular rejection and inflammation. Histologic i-, t-, and v-scores or molecular inflammation are actually lower in kidneys at risk of failure (probably due to scarring). The fact that v-lesions did not predict prognosis indicates changing concepts of risk.
To cite this abstract in AMA style:
Halloran PF. The Changing Face of T Cell-Mediated Rejection [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-changing-face-of-t-cell-mediated-rejection/. Accessed February 18, 2026.« Back to 2019 American Transplant Congress