TCMR in Late Kidney Transplant Biopsies Shows Less Molecular TCMR Activity and More Fibrosis Despite Persistence of Tubulitis and Interstitial Infiltrate
1Alberta Transplant Applied Genomics Centre, Edmonton AB, AB, Canada, 2., ., AB, Canada
Meeting: 2022 American Transplant Congress
Abstract number: 213
Keywords: Biopsy, Gene expression, Interferon (IFN), Rejection
Topic: Clinical Science » Kidney » 34 - Kidney: Acute Cellular Rejection
Session Information
Session Name: Kidney: Acute Cellular Rejection
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:30pm-4:40pm
Presentation Time: 4:30pm-4:40pm
Location: Hynes Ballroom A
*Purpose: We studied the relationship between time post-transplant and molecular T cell-mediated rejection (TCMR) activity in a population of indication kidney transplant biopsies.
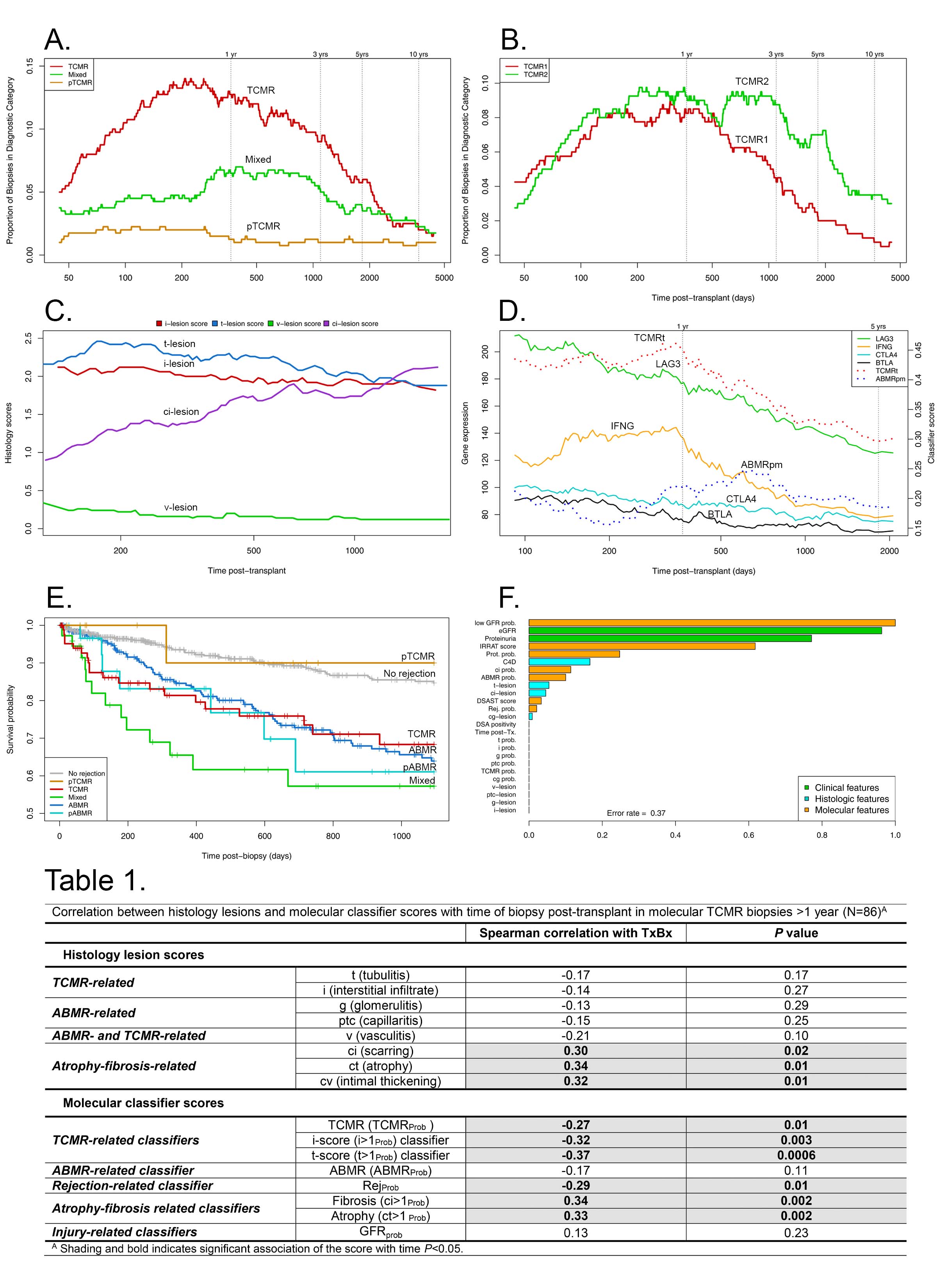
*Methods: Updated rejection-based principal component analysis (PCA) and archetypal analysis (AA) of genome-wide microarray results from 1679 kidney transplant biopsies (ClinicalTrials.gov #NCT01299168) generated two TCMR archetype scores: TCMR1 (N=75) and TCMR2 (N=100), totaling 175 TCMR biopsies.
*Results: We studied the frequency of TCMR and related molecular activity within the 175 TCMR biopsies. The frequency of molecular TCMR rose after 60 days, peaked and plateaued, then declined after 1000 days. Mixed rejection peaked about 500 days then declined (Fig 1A). The incidence of both TCMR1 and TCMR2 archetypes rose after two months, peaked at 6-12 months, and declined after three years (Fig 1B). Histologic interstitial infiltrate (i-score) and tubulitis (t-score) decreased slightly but remained at the diagnostic thresholds even in late TCMR. V-lesions declined but atrophy-fibrosis (ci lesions) increased (Fig 1C and Table 1). Within all archetypal TCMR biopsies, molecular effector T cell activation measures declined with time of biopsy post-transplant after 500 days: expression of T cell activation genes (e.g. IFNG, LAG3), IFNG-induced genes, and TCMR classifier scores (TCMRt, Fig 1D). Within TCMR, the ABMR score peaked about 500 days. TCMR was associated with as much impairment in survival at three years post-biopsy as ABMR (Fig 1E). However, within the TCMR biopsies, the variables in random forests most important for predicting graft failure by three years were the features of parenchymal injury, and were not tubulitis, v-lesions, or features of TCMR activity (Fig 1F). The lower TCMR activity in late TCMR suggests exhaustion of host cognate T cells. However, the decrease in TCMR activity over time was not related to increased biopsy expression of checkpoint genes, some of which significantly decreased in expression over time e.g. LAG3.
*Conclusions: TCMR declines in activity as well as frequency with time post-transplant >1000 days, suggestion exhaustion of host cognate T cell clones, and atrophy-fibrosis increases. Graft survival is reduced after TCMR biopsies, but this is related to parenchymal injury, not to TCMR activity.
To cite this abstract in AMA style:
Madill-Thomsen KS, Reeve J, Halloran P. TCMR in Late Kidney Transplant Biopsies Shows Less Molecular TCMR Activity and More Fibrosis Despite Persistence of Tubulitis and Interstitial Infiltrate [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/tcmr-in-late-kidney-transplant-biopsies-shows-less-molecular-tcmr-activity-and-more-fibrosis-despite-persistence-of-tubulitis-and-interstitial-infiltrate/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress