Taking on Pediatric Liver Tumors – Beyond Hepatoblastoma
MedStar Georgetown Transplant Institute, Washington, DC
Meeting: 2020 American Transplant Congress
Abstract number: B-143
Keywords: Liver transplantation, Malignancy, Outcome, Pediatric
Session Information
Session Name: Poster Session B: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Background. Hepatic angiosarcomas, hepatocellular carcinoma, hemangioendothelioma, and rhabdomyosarcoma of the bile ducts are very rare tumors in children with historically poor prognosis. Median survival following liver transplantation for hepatic angiosarcoma (HAS) is 6-months. Less than 20% of pediatric patients with hepatocellular carcinoma (HCC) are eligible for initial resection that is fundamental for cure. Infantile hepatic hemangioendothelioma (IHHE) can present with acute liver and heart failure in the postnatal period that complicates liver transplantation as a lifesaving option. Aims. We sought to describe our centers’ experience using liver transplantation as complementary therapy for hepatic angiosarcoma, hepatocellular carcinoma, hemangioendothelioma and rhabdomyosarcoma of the bile ducts in 6 children.
*Methods: We queried the database of Medstar Georgetown Transplant Institute (MGTI) for children who had undergone isolated liver transplantation for non-hepatoblastoma malignant liver tumors between August 2003 and November 2019, and described patient and graft outcomes.
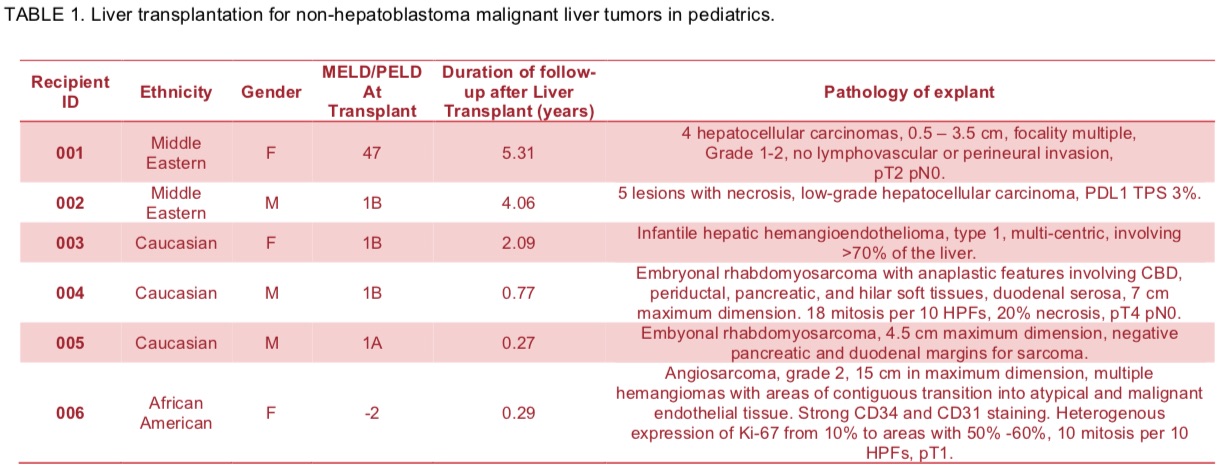
*Results: 6 children underwent 7 liver transplant procedures. 1 child underwent a liver re-transplant on POD #4 for hepatic artery thrombosis. 2 children each had a diagnosis of hepatocellular carcinoma, and rhabdomyosarcoma of the bile ducts; 1 child each had a diagnosis of hemangioendothelioma and hemangiosarcoma. The median age at transplant was 7.79-years (0.28 – 17.96). Pathology of the explant and duration of follow-up after liver transplantation is shown in Table 1. The 2 children with rhabdomyosarcoma underwent a Whipple procedure at time of liver transplant. Adjuvant chemotherapy was given to all patients peri-operatively. At the time of this report, all 6 children are alive with normal graft function and no tumor recurrence.
*Conclusions: There is an urgent need to develop pharmacologic treatments targeting angiogenic and non-VEGF angiogenic pathways to treat non-hepatoblastoma malignant liver tumors in children. Moreover, research has to be done to characterize the molecular and genomic mechanisms of these tumors to support the development of novel therapeutic approaches. In order to make progress, a combination of surgery, liver transplantation, anti-angiogenic and immunotherapy may be necessary.
To cite this abstract in AMA style:
Ekong U, Yazigi N, Khan K, Kaufman S, Guerra J, Girlanda R, Hawksworth J, Kroemer A, Matsumoto C, Fishbein T. Taking on Pediatric Liver Tumors – Beyond Hepatoblastoma [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/taking-on-pediatric-liver-tumors-beyond-hepatoblastoma/. Accessed March 7, 2026.« Back to 2020 American Transplant Congress