Staged Biliary Reconstruction after Liver Transplantation Reduces Post-Transplant Biliary Complications in High-Acuity Patients
Medical College of Wisconsin, Milwaukee, WI.
Meeting: 2018 American Transplant Congress
Abstract number: A240
Keywords: Bile duct, Liver transplantation, Post-operative complications
Session Information
Session Name: Poster Session A: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Biliary complications (BC) after liver transplantation (LT) are strongly associated with inferior patient outcomes and increased healthcare cost. High-acuity LT patients are at increased risk for BC. While a staged operative strategy in complex hepatobiliary surgery has improved post-operative outcomes, data on staged biliary reconstruction after LT (SBRALT) is limited. We sought to analyze the utility and outcomes of SBRALT in high-risk adult transplant recipients.
Methods: We conducted an analysis from our prospective database of 149 adult LTs at our center from January 2012 through June 2017. We compared Group I: single-stage LT with biliary anastomosis at the time of transplantation (n=58) vs Group II: two-stage LT with delayed biliary reconstruction (n=91).
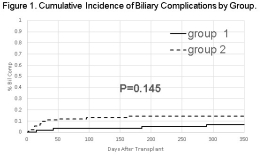
Results: Comparing Groups I and II: median age (53.3 vs 54.9 years), mean MELD scores (31.3 vs 34.7, P=0.002), MELD > 30 (57.7% vs 75.8%, P=0.021), patients requiring pre-transplant ICU (29.3% vs 54.9%, P=0.022), intraoperative renal replacement therapy (15.5% vs 48.4%, P<0.001), mean cold ischemia time (342.3 min vs 354.7 min), estimated blood loss (2879 mL vs 5989 mL, P<0.001), packed RBC transfusion (7.7 U vs 18.8 U, P<0.001), cryoprecipitate transfusion (1.8 U vs 7.0 U, P<0.001). Roux-en-Y hepaticojejunostomy was performed in 8.6% (Group I) and 25.3% (Group II), P=0.011. Compared to Group I, Group II had a significantly lesser amount of intraoperative blood loss (946 vs. 342 mL, P<0.001) and blood product transfusion (4.35 vs. 2.1 units, P<0.001) during the period of biliary reconstruction. For Groups I and II, one–year survival rates for graft (89.7% vs 88.2%, P=0.845) and patient (89.7% vs 88.2%, P=0.841) were comparable. Cumulative incidence of biliary complications for both groups were similar (Figure 1).
Conclusion: Our study shows a clear clinical benefit to staged biliary reconstruction after LT in high-risk transplant recipients. Two-stage LT with delayed biliary reconstruction is an acceptable operative strategy and can be applied to optimize outcomes in complex LT.
CITATION INFORMATION: Pearson T., Zimmerman M., Kim J., Palines P., Wong M., Erickson C., Hong J. Staged Biliary Reconstruction after Liver Transplantation Reduces Post-Transplant Biliary Complications in High-Acuity Patients Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Pearson T, Zimmerman M, Kim J, Palines P, Wong M, Erickson C, Hong J. Staged Biliary Reconstruction after Liver Transplantation Reduces Post-Transplant Biliary Complications in High-Acuity Patients [abstract]. https://atcmeetingabstracts.com/abstract/staged-biliary-reconstruction-after-liver-transplantation-reduces-post-transplant-biliary-complications-in-high-acuity-patients/. Accessed March 2, 2026.« Back to 2018 American Transplant Congress