Simultaneous Liver/ Kidney Transplant Reduces Both Donor Specific and Non-Donor Specific HLA Antibodies
Cedars Sinai Medical Center, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 932
Keywords: Antibodies, Histocompatibility, HLA antibodies, Kidney/liver transplantation
Topic: Basic Science » Basic Science » 11 - Histocompatibility and Immunogenetics
Session Information
Session Name: Histocompatibility and Immunogenetics
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Kidney allografts can be transplanted across strong donor specific antibody (DSA) barriers in simultaneous liver/kidney transplant (SLK) recipients. It is suggested that preformed DSAs can be reduced or eliminated via absorbance of DSA by the liver allograft. Recently, the SLK system was altered to provide a kidney safety net (SN) to those who do not recover kidney function after liver transplant. However, these kidneys provide additional challenges as their HLA antigens are not identical to the original liver graft. The goal of this study is to determine if the liver allograft in SLK can reduce HLA antibodies not against the HLA antigens of the liver graft.
*Methods: Between 2016 and 2020, 70 patients underwent SLK transplant and 8 patients underwent SN kidney transplant. The median time (interquartile range [IQR]) of post-transplant follow up was 883 days (459-1322).
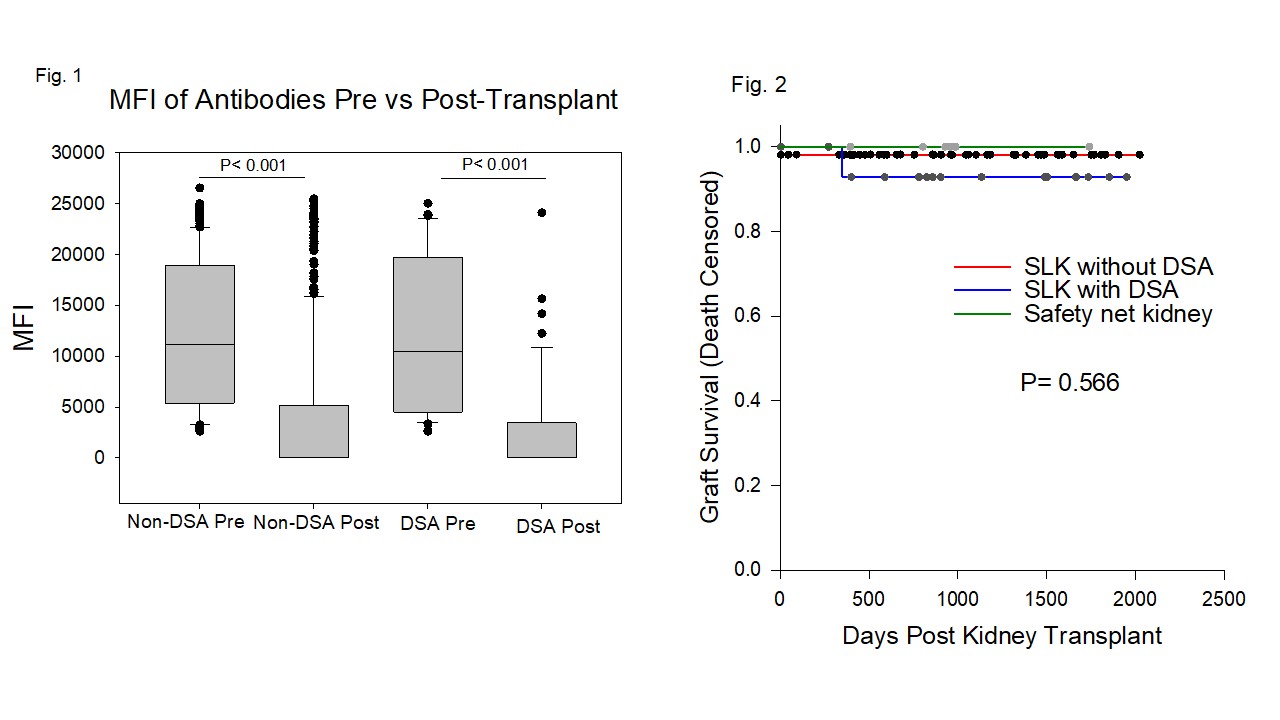
*Results: Of 70 SLK recipients, 4 recipients only had HLA antibodies tested pre-transplant, and 66 recipients had HLA antibodies tested on both pre and post-transplant samples with 33 of 66 demonstrating HLA antibodies pretransplant. MFI of DSAs were significantly reduced post SLK transplant in these 33 sensitized SLK patients. Of note, MFIs of non-DSA also decreased significantly post-transplant (Fig 1). 16 SLK recipients had DSA pretransplant: 9 recipients had strong preformed DSA (MFI>10,000), with 8 having ≥ 2 DSA; 2 recipients had moderate DSA (MFI >5,000); 5 recipients had weak DSA (MFI>2,500). Of these 16 recipients with preformed DSA, 14 recipients also had antibody tested posttransplant, and nearly all DSA became negative in 11 of 14 recipients by the first posttransplant test (The median time [IQR]: 27 days [16-62]). Levels of DSA were persistent in three recipients during the follow-up. The presence of preformed DSA in SLK recipients was not associated with kidney rejection, death-censored graft survival, or patient survival (p=0.167, p=0.361, p=0.999, respectively). 16 of 70 recipients underwent kidney biopsy, and two recipients who had persistent DSA were diagnosed with AMR. For SN transplant, 0 of 4 SN kidney recipients tested had HLA antibodies. When comparing SLK to SN kidney transplant, death-censored kidney graft survival was equivalent (p=0.566) (Fig. 2).
*Conclusions: Preformed DSAs are not associated with the patient and graft survival in SLK transplant. Levels of both DSA and non-DSA are reduced post SLK transplant, suggesting the liver transplant may reduce antibody levels via other mechanisms besides antibody absorbance, and the SN kidney transplant can also benefit from decreased antibodies by the previous liver transplant.
To cite this abstract in AMA style:
Zhang X, Wisel S, Kim I, Jordan S. Simultaneous Liver/ Kidney Transplant Reduces Both Donor Specific and Non-Donor Specific HLA Antibodies [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/simultaneous-liver-kidney-transplant-reduces-both-donor-specific-and-non-donor-specific-hla-antibodies/. Accessed February 22, 2026.« Back to 2022 American Transplant Congress