Risk Factors for Graft Failure in Kidney Transplant Recipients with Polycystic Kidney Disease
University of Wisconsin, Madison.
Meeting: 2018 American Transplant Congress
Abstract number: A140
Keywords: Graft failure, Kidney transplantation, Polycystic kidney disease
Session Information
Session Name: Poster Session A: Kidney Complications: Late Graft Failure
Session Type: Poster Session
Date: Saturday, June 2, 2018
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall 4EF
Background: Polycystic kidney disease (PKD) is the underlying renal disease in 15% of kidney transplant recipients (KTRs) in the US. Post-transplant outcomes and contributing factors in PKD recipients are unclear with varying results reported in prior studies.
Methods: We compared outcomes (adjusted for baseline characteristics) in consecutive KTRs with PKD vs. other native renal diseases (non-PKD) at our center between 1/1/1994-6/30/2014. In PKD KTRs, we evaluated factors influencing outcomes in a multivariate analysis.
Results: We identified 619 PKD and 4,312 non-PKD KTRs. Pertinent baseline characteristics are shown.
| Baseline characteristic (units) | PKD (N=619) | Non-PKD (N=4312) | P-Value |
| Age (years) | 52.9 (+9.13) | 48.7 (+13.4) | <0.01 |
| Female (%) | 45.7 | 39.3 | <0.01 |
| Non-White Race (%) | 6.6 | 17.2 | <0.01 |
| Any dialysis prior to transplant (%) | 60.1 | 78.3 | <0.01 |
| Delayed graft function (DGF; %) | 14.7 | 19.1 | <0.01 |
| Calcineurin inhibitor use (CNI; %) | 90.8 | 90.7 | 0.93 |
| HLA mismatch>2 (%) | 76.4 | 71.2 | <0.01 |
| cPRA>10% (%) | 23.3 (N=296) | 30.8 (N=2088) | <0.01 |
| Native nephrectomy at transplant (%) | 26.8 | 0.9 | <0.01 |
Patient survival and allograft longevity were better in PKD group (HR for death=0.55;[0.46-0.66; P<0.001]; HR for death-censored graft loss=0.75; 95% CI:[0.61-0.93; P=0.010]). There was no difference in acute rejection between PKD and non-PKD recipients. 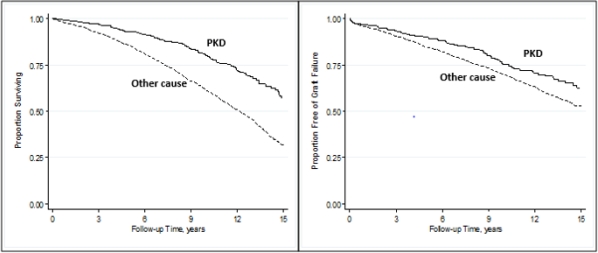
Cox regression identified 3 independent risk factors for death censored graft loss in PKD KTRs: CNI use (HR=0.47;[0.28-0.77; p=0.003]), >2 HLA mismatch (HR=1.90;[1.16-3.1; p=0.01]) and DGF (HR=1.78;[1.10-2.91; p=0.02]). Native nephrectomy at transplant was not associated with graft failure (HR=1.02[0.66-1.58; p=0.914]).
Discussion: Our study shows that recipients with PKD have better graft and patient outcomes compared to recipients with other native renal disease. While native nephrectomy was not associated with graft survival, HLA matching, and CNI use were modifiable risk factors, which predicted improved graft survival in PKD recipients.
CITATION INFORMATION: Bhutani G., Astor B., Djamali A. Risk Factors for Graft Failure in Kidney Transplant Recipients with Polycystic Kidney Disease Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Bhutani G, Astor B, Djamali A. Risk Factors for Graft Failure in Kidney Transplant Recipients with Polycystic Kidney Disease [abstract]. https://atcmeetingabstracts.com/abstract/risk-factors-for-graft-failure-in-kidney-transplant-recipients-with-polycystic-kidney-disease/. Accessed July 5, 2025.« Back to 2018 American Transplant Congress
