Risk Factors Associated with Hepatic Artery Thrombosis in the Modern Era
Johns Hopkins, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: B-150
Keywords: Graft failure, Hepatic artery, Liver transplantation
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Historically, hepatic artery thrombosis (HAT) has been associated with certain risk factors, such as donor age, cold ischemia time, and split grafts; it is unclear how the increased use of marginal donors has influenced HAT incidence. We investigated potential donor, recipient, and graft risk factors for HAT in the modern era.
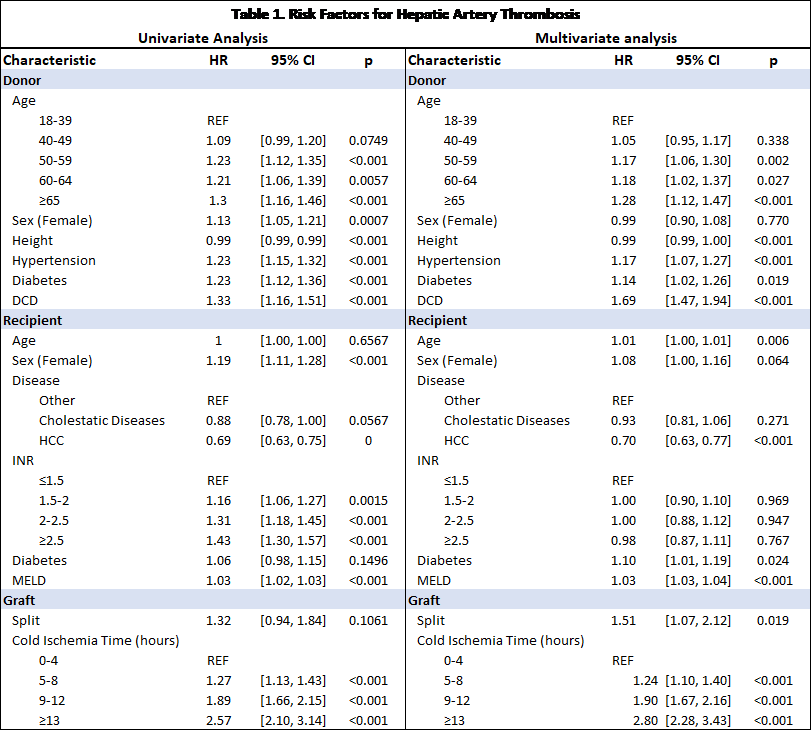
*Methods: We used SRTR data from January 2006- March 2019 to identify first-time adult deceased donor liver transplant recipients. HAT was defined by graft failure or death due to vascular thrombosis within 90 days of transplant. We used cox regression to quantify the risk of HAT, adjusting for characteristics of the donor (age, gender, height, hypertension, diabetes, DCD), recipient (age, gender, disease, INR, diabetes, MELD) and graft (cold ischemia time, split).
*Results: Risk factors for HAT included both donor and recipient characteristics (Table 1). After adjustment, there was a progressive relationship between donor age (hazard ration (HR) for donor age 40-49: 0.951.051.17, age 50-59: 1.061.171.30, age 60-65: 1.021.181.37, older than 65: 1.121.281.47; Figure 1). Similarly, cold ischemia time was related to HAT, HR for 5-8 hours: 1.101.241.40, 9-12 hours: 1.671.902.16, more than 13 hours: 2.283.803.43. DCD livers were associated with HAT (HR 1.471.691.94) as were split grafts (1.071.512.12). Patients with HCC had a significantly reduced chance of HAT compared to other indications for liver transplant (HR 0.630.700.77), while those with cholestatic diseases had no significant change in risk (HR 0.810.931.06).
*Conclusions: No contemporary evaluations of risk factors for HAT have been done to date. Using national registry data, we have reaffirmed known risk factors and highlighted additional associations for HAT. Notably, a patient’s indication for liver transplant appears to be an important factor in predicting the risk of development of HAT after transplantation.
To cite this abstract in AMA style:
Krach M, Kernodle A, Chiang P, Segev D, Massie A, Garonzik-Wang J. Risk Factors Associated with Hepatic Artery Thrombosis in the Modern Era [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/risk-factors-associated-with-hepatic-artery-thrombosis-in-the-modern-era/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress