Renal Graft Survival According to Banff 2013 Diagnostic Categories in Indication Biopsies.
1Nephrology, Hospital del Mar, Barcelona, Spain
2Pathology, Hospital del Mar, Barcelona, Spain.
Meeting: 2016 American Transplant Congress
Abstract number: A236
Keywords: Biopsy, Graft survival, Kidney transplantation
Session Information
Session Name: Poster Session A: Long Term Outcomes in Kidney Transplantation
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
The impact of acute rejection in kidney graft survival is well known, but the prognosis of other diagnosis is uncertain. We evaluated the frequency and impact on graft survival of different diagnostic categories according to the Banff'2013 classification in a cohort of renal transplant recipients. Retrospective study of 495 indication biopsies in 322 renal transplant recipients during the years 1990-2014. Two independent observers reviewed the histological reports, reclassifying according to Banff-2013 classification.
Among the 495 biopsies, 28 (5.7%) were not diagnostic. Among the remaining 467, 10.3% were "normal" (category 1), 19.6% showed antibody-mediated changes (category 2), 5.9%"borderline" changes (category 3), 8.7% T-cell mediated rejection (category 4), 23.4% interstitial fibrosis/tubular atrophy (IFTA) (category 5), and 26.5% other diagnoses (category 6). When increasing the time after transplantation, diagnostic categories 1, 3 and 4 decrease in frequency and categories 2 and 5 increase. Compared with category 1 (Normal), a worse graft survival was observed with diagnoses of category 2 (45% at 7.5 years, HR 4.29 for graft loss [95% CI 2.39-7.73]; p<0.001) or category 5 (HR 2.41, CI 1.36-4.27, p=0.003). A diagnosis of acute T-cell rejection was unrelated to graft survival (HR 0.98, CI 0.90-3.49, p=0.98), 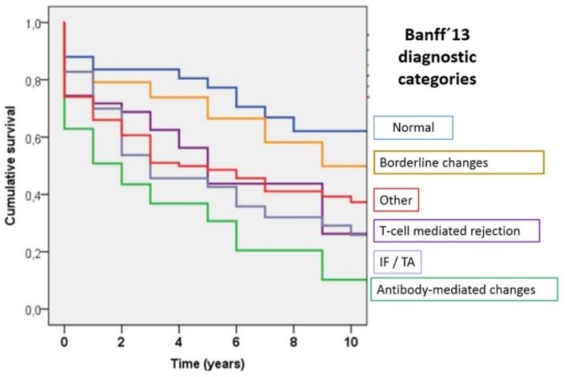 . Allografts with “unfavorable histology" (chronic antibody-mediated rejection, moderate-severe IFTA) compared with allograft with "favorable histology" (normal biopsy, acute tubular necrosis, mild IFTA), have worst survival rates (p<0.001).
. Allografts with “unfavorable histology" (chronic antibody-mediated rejection, moderate-severe IFTA) compared with allograft with "favorable histology" (normal biopsy, acute tubular necrosis, mild IFTA), have worst survival rates (p<0.001).
Banff 2013 classification allows a histological diagnosis in 95% of indication biopsies. While diagnostic category 6 is the most common, we can see a modification in the predominant histopathology according to time of transplantation. Antibody-mediated changes are associated with worse graft survival but T-cell mediated rejection does not impact on outcomes.
CITATION INFORMATION: Redondo-Pachón D, Arias-Cabrales C, Pérez-Sáez M, Gimeno J, Sánchez-Güerri I, Bermejo S, Sierra A, Burballa C, Mir M, Crespo M, Pascual J. Renal Graft Survival According to Banff 2013 Diagnostic Categories in Indication Biopsies. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Redondo-Pachón D, Arias-Cabrales C, Pérez-Sáez M, Gimeno J, Sánchez-Güerri I, Bermejo S, Sierra A, Burballa C, Mir M, Crespo M, Pascual J. Renal Graft Survival According to Banff 2013 Diagnostic Categories in Indication Biopsies. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/renal-graft-survival-according-to-banff-2013-diagnostic-categories-in-indication-biopsies/. Accessed February 21, 2026.« Back to 2016 American Transplant Congress
