Regulatory T Cells Suppress Memory IL-17a Production in Highly Sensitised Patients with End-Stage Renal Disease
1King's College London, London, United Kingdom, 2Viapath Clinical Transplantation Laboratory, Guy's Hospital, London, United Kingdom
Meeting: 2022 American Transplant Congress
Abstract number: 1257
Keywords: Alloantibodies, Highly-sensitized, Kidney transplantation, T cells
Topic: Basic Science » Basic Science » 10 - Treg/Other Regulatory Cell/Tolerance
Session Information
Session Name: Treg/Other Regulatory Cell/Tolerance
Session Type: Poster Abstract
Date: Monday, June 6, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Highly sensitised patients exhibit poorer long-term outcomes following renal transplantation compared to those non sensitised individuals. IL17-A has been associated with acute rejection. Presence of regulatory T cells (Tregs) has been associated with regulation in patients with chronic rejection. Therapy using autologous expanded Tregs has been demonstrated to be safe. This project aims to test the hypothesis that Tregs could be used in sensitised patients to suppress memory IL-17A responses.
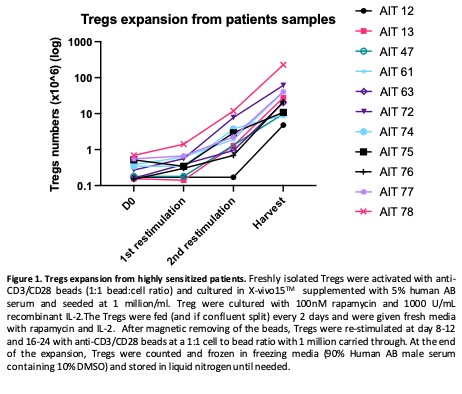
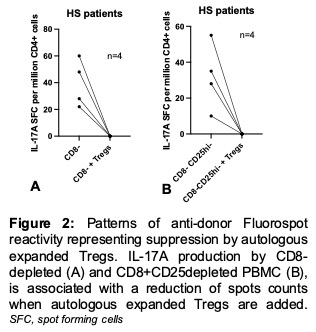
*Methods: We prospectively recruited highly-sensitised patients on haemodialysis, isolated their Tregs and expanded them using established protocols (Interleukin-2 + Rapamycin). IL-17A production by CD8-depleted peripheral blood mononuclear cells (PBMC)(+/- additional depletion of CD25hi cells) in response to Human Leucocyte Antigen (HLA) proteins (PureProt®) was tested in FluoroSpot to assess the memory immune alloresponses at baseline and when expanded autologous Tregs were also added.
*Results: Of the patients included, 10/16 were sensitised by previous renal transplant and of those 4/10 had had nephrectomy. 4/10 (40%) of post-transplant patients were on immunosuppression. We managed to expand Tregs for 11/16 (69%) patients (Figure 1). Five/11 (45%) patients had spontaneous IL-17A production in CD8-depleted PBMCs challenged with an HLA protein that they had been sensitised to (Figure 2). In 4/5 patients (80%), IL-17A production was reduced when autologous ex vivo expanded Tregs were added. Moreover, in 6/11 (55%) patients, CD8-CD25hi- PBMCs stimulated with pure HLA protein were associated with IL-17A production, which was suppressed in 4/6 when expanded autologous Tregs were also added.
*Conclusions: Forty-five percent of HS patients made IL-17A when challenged by an HLA protein they have made an HLA antibody against. In most of these patients, IL-17A could be inhibited by autologous ex vivo expanded Tregs. The Phase IIa trial GAMECHANgER-1 will test whether these findings are reproducible in vivo in HS patients awaiting renal transplantation.
To cite this abstract in AMA style:
Dudreuilh C, Basu S, Shaw O, Burton H, Domingo-Vila C, Tree T, Lombardi G, Scotta C, Dorling A. Regulatory T Cells Suppress Memory IL-17a Production in Highly Sensitised Patients with End-Stage Renal Disease [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/regulatory-t-cells-suppress-memory-il-17a-production-in-highly-sensitised-patients-with-end-stage-renal-disease/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress