Recipient Monocytes Activated by Endobronchial Toll-Like Receptor 2 Agonist Prevent Tolerance Induction after Lung Transplantation
1Department of Surgery, Washington University in St. Louis, St. Louis, MO, 2Department of Surgery, The University of Virginia, Charlottesville, VA
Meeting: 2019 American Transplant Congress
Abstract number: A23
Keywords: Lung transplantation, Mononuclear leukocytes, Rejection, T cell activation
Session Information
Session Name: Poster Session A: Acute Rejection
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Extended criteria lung donors are being increasingly utilized, raising the possibility of transplanting lungs with a pre-existing pneumonia; how donor pneumonia alters alloimmune responses, however, is not well understood. We recently uncovered the critical role of recipient-derived monocytes in mediating ischemia-reperfusion injury in a mouse lung transplant model. Here, we test the hypothesis that recipient-derived monocytes activated by Toll-like receptor 2 (TLR2) agonist Pam3Cys4, a synthetic bacterial lipopeptide, can alter alloimmune responses following lung transplantation.
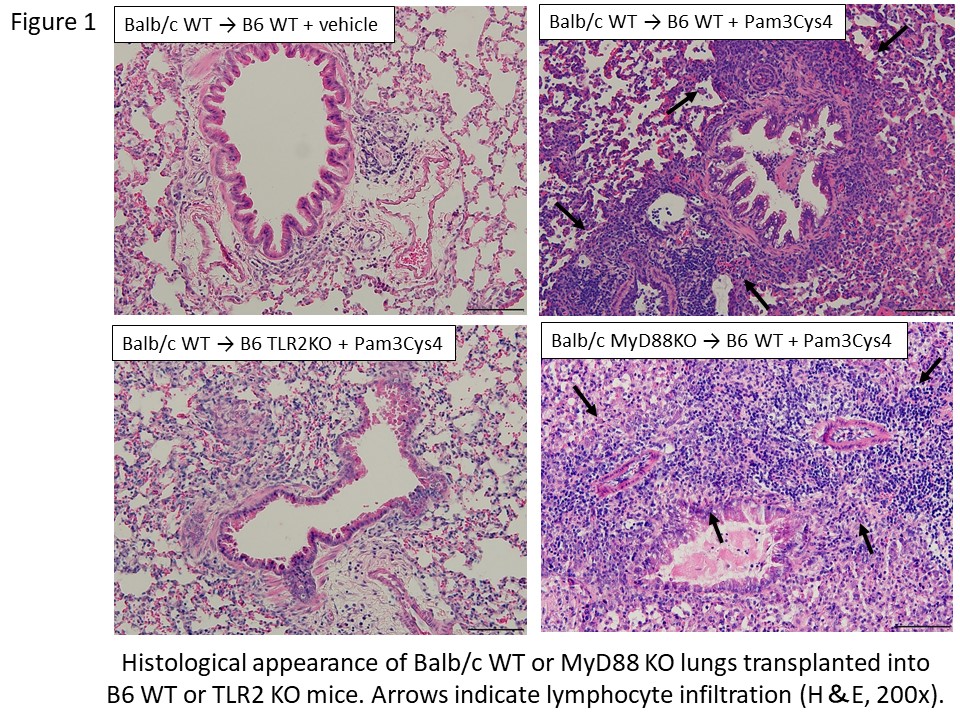
*Methods: Lungs from Balb/c wild type (WT) or Balb/c MyD88 KO were transplanted into B6 WT or B6 TLR2 KO recipients under perioperative co-stimulatory blockade (anti-CD40L at day 0 and CTLA4-Ig at day 2). Pam3Cys4 (50μg) or vehicle were administered into the donor bronchus prior to airway anastomosis in all transplants. For adoptive transfer experiments, T cells or monocytes were isolated from B6 WT mice and intravenously injected into recipient mice just after reperfusion. Lung grafts were harvested on day 7 and evaluated with histology and flow cytometry.
*Results: Balb/c WT lung grafts treated with vehicle and transplanted in B6 WT did not show rejection (Grade A0-A1, n=4). When treated with Pam3Cys4, Balb/c WT and Balb/c MyD88 KO lung grafts transplanted into B6 WT mice developed acute cellular rejection (Grade≥A2, n=4-5/group); however, Balb/c WT lung grafts transplanted in B6 TLR2 KO mice were not rejected (Grade A0-A1, n=5/group) (Figure 1). Rejection was associated with increased abundance of interstitial macrophages, lower CD4/CD8 ratio, and increased expression of Ki67 in CD8+ T cells (p<0.05) within the lung grafts. Adoptive transfer of B6 WT monocytes, but not T cells, following Balb/c WT→B6 TLR2 KO transplants triggered acute cellular rejection (Grade≥A2, n=4).
*Conclusions: Activation of TLR2 by a bacterial lipopeptide present within the donor airway prevents the induction of lung allograft tolerance through a process mediated by recipient-derived monocytes. Our work suggests that donor lungs harboring pneumonia may precipitate an inflammatory response and facilitate allograft rejection.
To cite this abstract in AMA style:
Tanaka S, Gauthier JM, Terada Y, Takahashi T, Li W, Higashikubo R, Tong AY, Puri V, Krupnick AS, Gelman AE, Kreisel D. Recipient Monocytes Activated by Endobronchial Toll-Like Receptor 2 Agonist Prevent Tolerance Induction after Lung Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/recipient-monocytes-activated-by-endobronchial-toll-like-receptor-2-agonist-prevent-tolerance-induction-after-lung-transplantation/. Accessed February 28, 2026.« Back to 2019 American Transplant Congress