PTLD Suspected by Visualization of Atypical Urinary Lymphocytes
J. Huidobro E1, F. Anghileri2, P. Troncoso3, A. Huete4, P. Downey1
1Nephrology, Pontificia Universidad Catolica de Chile, Santiago, Chile, 2Clinical Laboratories, Pontificia Universidad Catolica de Chile, Santiago, Chile, 3Urology, Pontificia Universidad Catolica de Chile, Santiago, Chile, 4Radiology, Pontificia Universidad Catolica de Chile, Santiago, Chile
Meeting: 2022 American Transplant Congress
Abstract number: 1013
Keywords: Epstein-Barr virus (EBV), Lymphocytes, Post-transplant lymphoproliferative disorder (PTLD), Urinalysis
Topic: Clinical Science » Infection Disease » 28 - PTLD: All Topics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Urinalysis has been used for the detection of acute rejection but visualization of atypical lymphocytes in the urine sediment as an early sign of post-transplant lymphoproliferative disease (PTLD) has not been described.
*Methods: We report the case of a 39 y/o woman with kidney failure secondary to lupus nephritis for which she received an unrelated living donor kidney transplant (KT). cPRA was 54% and flow cytometry crossmatch was negative. She and her donor were EBV IgG positive. The patient received thymoglobulin and steroids for induction but after reaching normal creatinine, she developed acute antibody-mediated rejection. She was treated with plasmapheresis, immunoglobulin and rituximab. Bortezomib was added due to lack of response. Creatinine was 1.47 mg/dL after treatment and the patient was discharged with cyclosporine, everolimus and prednisone.
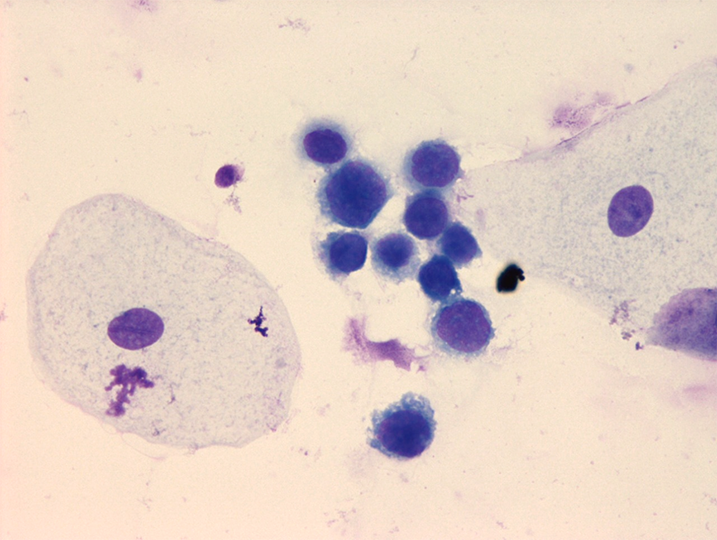
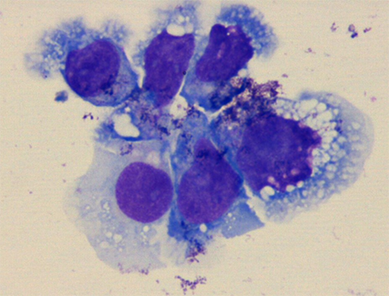
*Results: Seven months after KT urinalysis showed normal and atypical lymphocytes (figs. 1 & 2, respectively). One month later creatinine rose to 5.6 mg/dL. Allograft doppler US was normal. Kidney biopsy showed no signs of acute rejection. Due to persistence of graft dysfunction a CT scan and MRI were performed, showing a hilar pelvic mass. Ureteral stent was placed, and biopsy obtained by ureteroscopy confirmed monomorphic PTLD (large B cells) EBV (+) with flow cytometry compatible with B-cell PTLD. She was treated with R-CHOP and creatinine dropped to 1.34 mg/dL.
*Conclusions: PTLD is a serious complication after KT. Clinical presentation is variable, but early-onset PTLD more frequently are EBV positive and have graft involvement. Early diagnosis of PTLD is crucial to prognosis. Urinalysis has been reported useful in the detection of acute rejection, specially using flow cytometry. In this case, visualization of atypical urinary lymphocytes raised the suspicion of urinary tract PTLD, allowing prompt diagnosis and management. We report this case to highlight the importance of urinary sediment analysis in the follow-up of KT recipients.
To cite this abstract in AMA style:
E JHuidobro, Anghileri F, Troncoso P, Huete A, Downey P. PTLD Suspected by Visualization of Atypical Urinary Lymphocytes [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/ptld-suspected-by-visualization-of-atypical-urinary-lymphocytes/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress