Proinflammatory Cytokines Including IL-18 Correlate with Cytomegalovirus DNAemia in Solid Organ Transplant Recipients
A. H. Karaba, A. Figueroa, S. C. Ray, R. K. Avery, A. L. Cox
Division of Infectious Diseases, Department of Medicine, Johns Hopkins University, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: C-181
Keywords: Cytomeglovirus, Inflammation
Session Information
Session Name: Poster Session C: All Infections (Excluding Kidney & Viral Hepatitis)
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Human cytomegalovirus (CMV) is a common immunomodulatory virus that still causes significant morbidity and mortality in solid organ transplant (SOT) recipients despite prophylaxis. Cytokines are signaling molecules which help shape the immune response to the virus. While a number of cytokines increase during CMV DNAemia in SOT recipients, studies have largely focused on D+/R- recipients who are at the highest risk of disease. Furthermore, IL-18, a product of an innate sensing pathway called the inflammasome, is generally not assessed in these studies. We have previously found that plasma IL-18 levels correlate well with viremia and disease in HIV and hepatitis C virus (HCV). The purpose of this study was to determine whether IL-18 and other proinflammatory cytokine levels correlate with CMV DNAemia and disease severity.
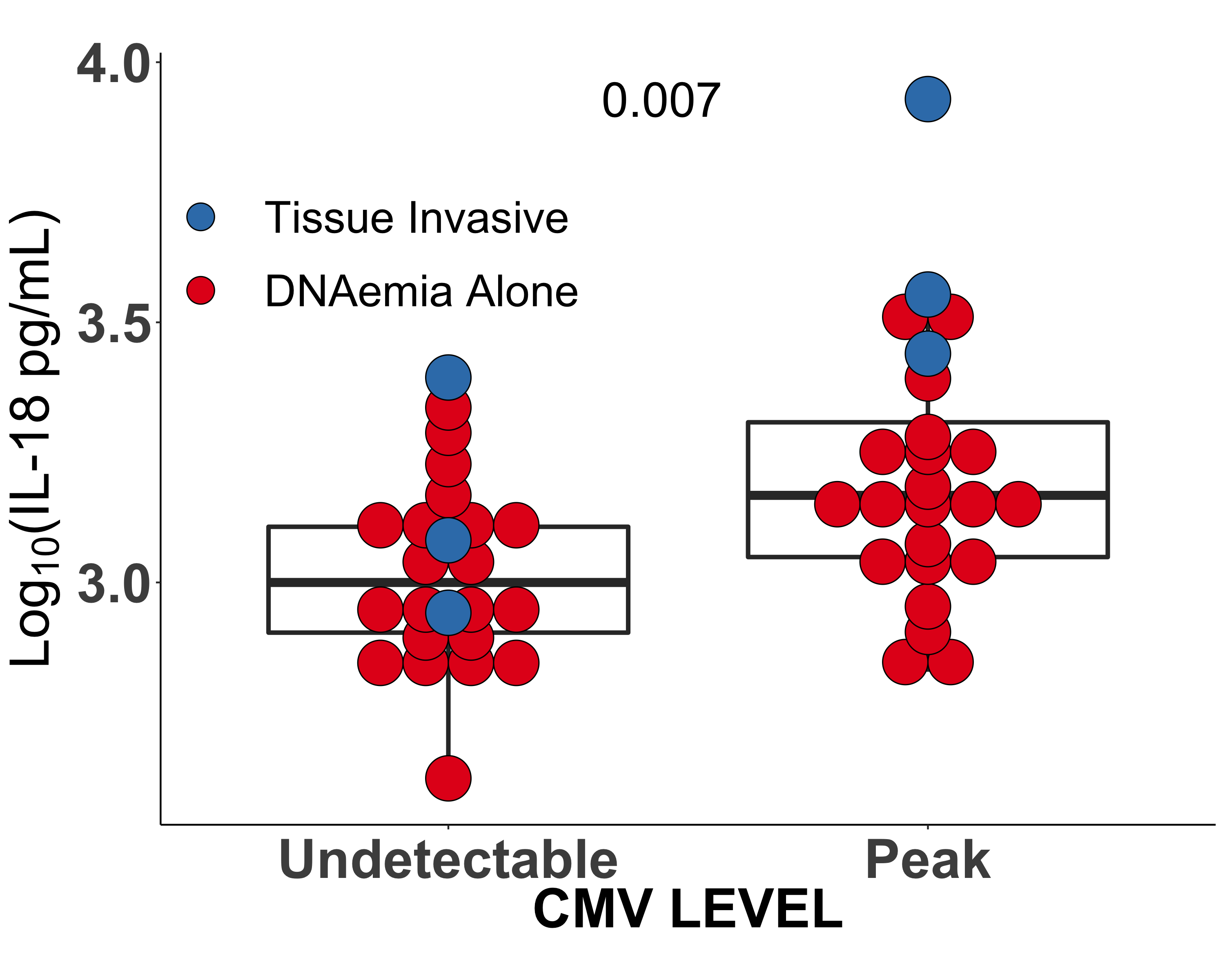
*Methods: Eleven cytokines (IFNγ, TNFα, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, IL-13, IL-18) were measured in residual plasma from 23 SOT recipients (2 heart, 11 kidney, 6 lung, 3 liver, 2 liver/kidney) with CMV DNAemia using a commercially available multiplex assay. Cytokines were measured at peak CMV DNA and in samples from the same subjects with undetectable CMV DNA, and the results were compared using a paired Wilcoxon test. Additionally, multiple linear regression analysis was used to assess correlations between cytokine and CMV DNA levels.
*Results: Among the eleven cytokines measured, six were significantly increased during peak CMV DNAemia (range 38.7 IU/mL to 43,000 IU/mL) compared to samples from the same subject with undetectable CMV (IFNγ, IL-10, IL-12p70, IL-18, IL-2, and TNFα) (p < 0.05). In the R+ subgroup the same six cytokines were significantly elevated during peak CMV DNAemia. In the R- subgroup the trend was similar, but the difference did not reach statistical significance. When CMV was undetectable in plasma, IL-10 was significantly increased in the R+ group compared to R- (1.19 pg/mL vs. 0.559 pg/mL, p = .007). Elevations in four of the cytokines were significantly associated with increases in CMV DNA (adjusted R2 value of 0.4 and p-value of 1×10-15). Furthermore, high levels of IL-18 were associated with tissue invasive disease (n = 3 for patients with tissue invasive disease, see figure).
*Conclusions: IL-18 increases during periods of CMV DNAemia among SOT recipients regardless of graft type and recipient serostatus. This may be a useful marker of more severe disease, and further investigation into the role this inflammasome associated cytokine in CMV disease is warranted.
To cite this abstract in AMA style:
Karaba AH, Figueroa A, Ray SC, Avery RK, Cox AL. Proinflammatory Cytokines Including IL-18 Correlate with Cytomegalovirus DNAemia in Solid Organ Transplant Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/proinflammatory-cytokines-including-il-18-correlate-with-cytomegalovirus-dnaemia-in-solid-organ-transplant-recipients/. Accessed February 25, 2026.« Back to 2020 American Transplant Congress