Prevalence of Cutaneous Disease in Solid Organ Transplant Recipients: A 5-Year Study from a Medical -Surgical Transplant Dermatology Center.
Dermatology, Drexel University College of Medicine, Philadelphia, PA
Meeting: 2017 American Transplant Congress
Abstract number: B111
Keywords: Fungal infection, Malignancy, Quality of life
Session Information
Session Name: Poster Session B: Bacteria, Fungi, Parasites
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Background: Solid organ transplant recipients (OTR) on chronic immunosuppression exhibit heightened risk of developing a myriad of cutaneous manifestations compared to non-transplant patients, including cutaneous malignancy, atopic dermatitis, superficial fungal infections, benign skin growths and folliculitis. The prevalence of cutaneous disease in OTR is underreported in both the dermatology and transplant literature. Our study reports the 5-year prevalence of dermatologic conditions diagnosed in a specialty medical-surgical transplant dermatology clinic.
Methods: A retrospective chart review of 427 OTR evaluated in the Drexel Dermatology Center for Transplant Patients from 11/1/11 to 10/31/16.
Results: Benign growths were diagnosed in 31.1% (N=128) of patients, followed by fungal infection (N=20.4%, N=84), and malignancy (17.0%, N=70). Malignancy included basal cell carcinoma, squamous cell carcinoma, and melanoma. Fungal infections included candidiasis, dermatophytosis and pityrosporum/malassezia infections. Viral infections (13.3%, N=55) included human papillomavirus, herpes simplex virus, and trichodysplasia spinulosa. Additional notable categories were acne/folliculitis (18.0%, N=74), papulosquamous dermatoses (11.9%, N=49), premalignant lesions (10.0%, N=41), pigmentary disorders (8.0%, N=33), and autoimmune dermatoses (4.1%, N=17). 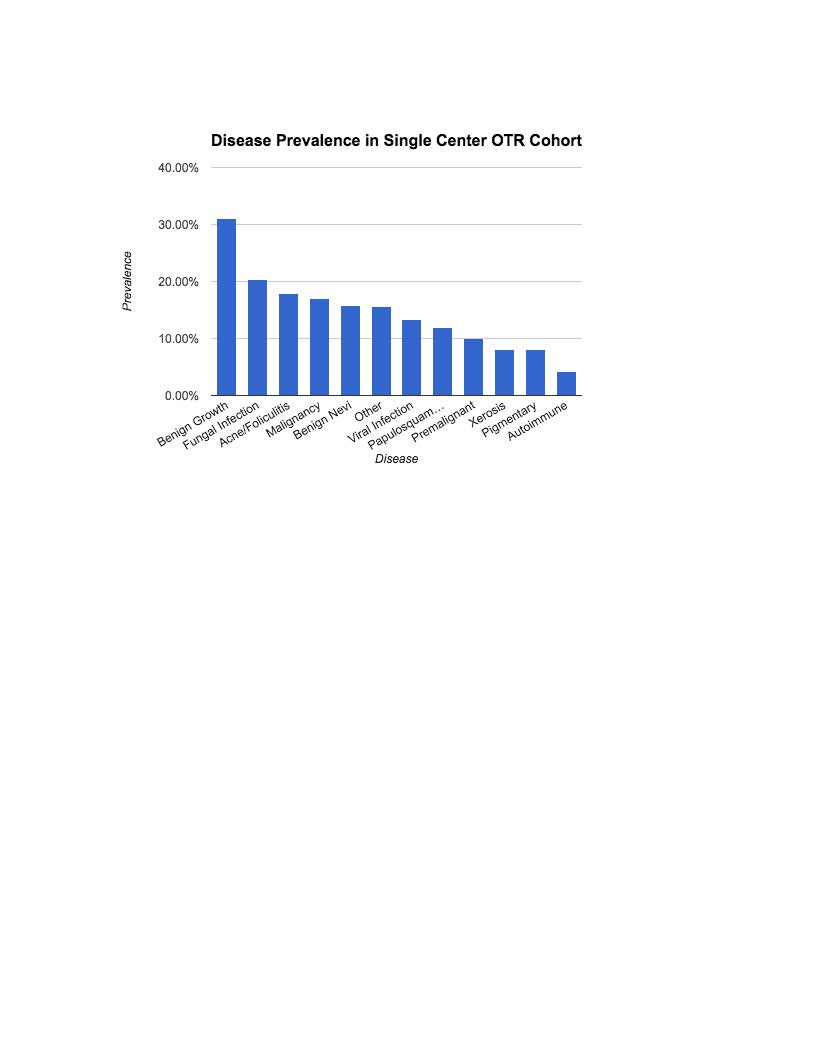 Conclusion: The most commonly diagnosed disease processes in our OTR cohort were infectious conditions including fungal and viral infections followed by cutaneous malignancy. Papulosquamous dermatoses and autoimmune conditions were also frequently diagnosed. Our study underscores the importance of increased awareness of posttransplant cutaneous disease among dermatologists and transplant physicians. Comprehensive posttransplant dermatologic care delivered in a multidisciplinary medical-surgical specialty clinic is essential in the prevention, early diagnosis, and management of cutaneous malignancy and skin disease in the organ transplant population.
Conclusion: The most commonly diagnosed disease processes in our OTR cohort were infectious conditions including fungal and viral infections followed by cutaneous malignancy. Papulosquamous dermatoses and autoimmune conditions were also frequently diagnosed. Our study underscores the importance of increased awareness of posttransplant cutaneous disease among dermatologists and transplant physicians. Comprehensive posttransplant dermatologic care delivered in a multidisciplinary medical-surgical specialty clinic is essential in the prevention, early diagnosis, and management of cutaneous malignancy and skin disease in the organ transplant population.
CITATION INFORMATION: Allawh R, Weiffenbach A, Nadhan K, Abdelmalek M, Cusack C, Chung C. Prevalence of Cutaneous Disease in Solid Organ Transplant Recipients: A 5-Year Study from a Medical -Surgical Transplant Dermatology Center. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Allawh R, Weiffenbach A, Nadhan K, Abdelmalek M, Cusack C, Chung C. Prevalence of Cutaneous Disease in Solid Organ Transplant Recipients: A 5-Year Study from a Medical -Surgical Transplant Dermatology Center. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/prevalence-of-cutaneous-disease-in-solid-organ-transplant-recipients-a-5-year-study-from-a-medical-surgical-transplant-dermatology-center/. Accessed July 2, 2025.« Back to 2017 American Transplant Congress
