Prevalence and Clinical Outcomes in Kidney Transplant Patients with Viral and Fungal Opportunistic Infections and Malignancy.
Montefiore Medical Center, Bronx
Meeting: 2017 American Transplant Congress
Abstract number: A207
Keywords: Graft survival, Infection, Malignancy
Session Information
Session Name: Poster Session A: Kidney Complications I
Session Type: Poster Session
Date: Saturday, April 29, 2017
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall D1
Opportunistic infections and malignancy after kidney transplant (KTX) are associated with increased morbidity and mortality. We aimed to assess predictors and clinical outcomes in patients with these complications.
We performed a single-center retrospective review of KTX patients from January 2009 until December 2014. Patients with opportunistic viral infections (BKV or CMV), fungal infections, or malignancies were reviewed and compared to patients without these complications.
During a median follow-up of 3.8 years (2.4-5.3), of 673 patients, 226 developed opportunistic infection/malignancy (34%); 19.8% had BKV, 1.9% BK nephropathy, 9.6% CMV, 2.1% invasive CMV infection, 2.2% fungal infection, and 5.8% had malignancies. There was no difference between the groups in terms of age (52.5±13.4 vs. 54.7 ±13), African American race (42.6% vs. 39.6%), induction type (anti-thymocyte globulin 59% vs. 56%), etiology of kidney disease (DM 24.2% vs. 26.2%), patients with PRA >20% (class I 23.5% vs. 26.6%, class II 25.2% vs. 25.5%) or with pre-KTX DSA (15.4% vs.16.7%), however, more patients with infection/malignancy were male (64.7% vs. 56.4% p=0.04). Patients received kidneys from donors with similar mean KDPI score (60.3±26.8 vs. 63.3±27.3) and with similar terminal creatinine (1.49±1.22mg/dl vs. 1.56±1.27mg/dl), however, more patients with infection/malignancy received deceased donor KTX (81% vs. 74% p=0.01), from older donors (age 45.4±15.5 vs. 42.6±15.2 p=0.01) with longer cold ischemia times (1354±868.4 vs. 1159±874.1 p<0.01). There was no difference in acute rejection episodes (14% vs. 9%), development of recurrent or de novo glomerular disease (8.1%vs. 6.1%) or transplant glomerulopathy (7.6% vs. 8.8%). Development of de novo DSA was not different between the two groups (17.3% versus 14.7%). Most recent serum creatinine levels were higher in the infection/malignancy group (1.6±0.75mg/dl vs. 1.5±1.1mg/dl p<0.01), however, there was no difference in graft or patient survival between the two groups.
While opportunistic infections and malignancies develop in 34% of kidney transplant recipients, it does not effect patient and graft survival.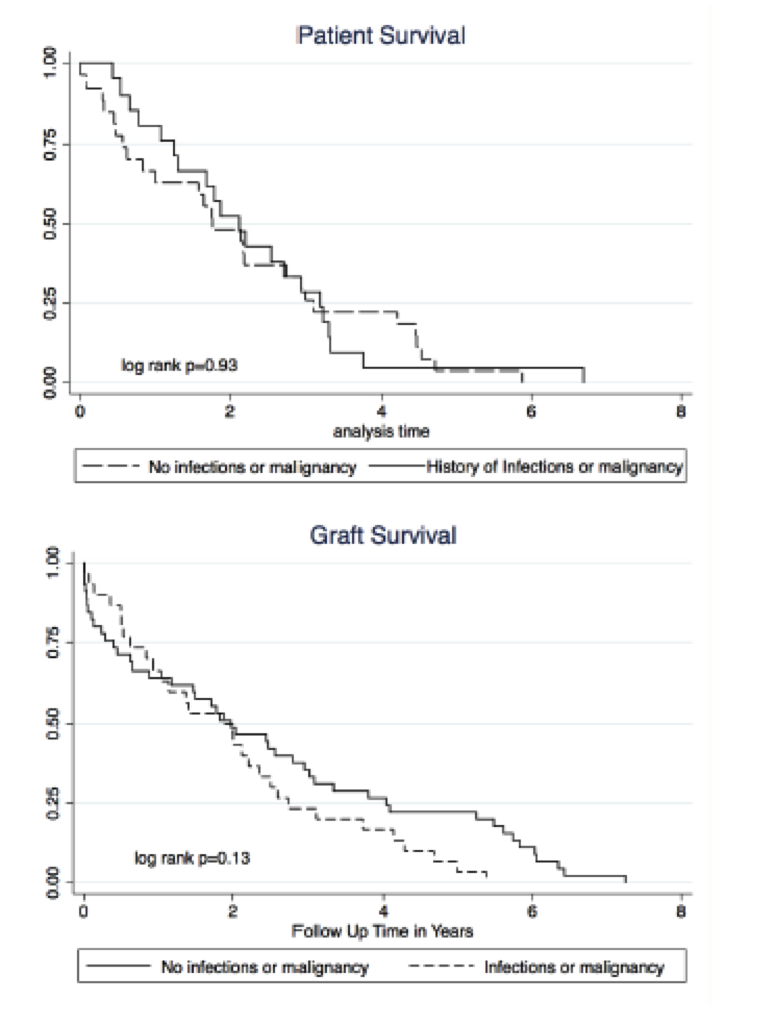
CITATION INFORMATION: Lubetzky M, Hayde N, Kamal L, Ajaimy M, Bedi P, Deboccardo G, Akalin E. Prevalence and Clinical Outcomes in Kidney Transplant Patients with Viral and Fungal Opportunistic Infections and Malignancy. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Lubetzky M, Hayde N, Kamal L, Ajaimy M, Bedi P, Deboccardo G, Akalin E. Prevalence and Clinical Outcomes in Kidney Transplant Patients with Viral and Fungal Opportunistic Infections and Malignancy. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/prevalence-and-clinical-outcomes-in-kidney-transplant-patients-with-viral-and-fungal-opportunistic-infections-and-malignancy/. Accessed February 21, 2026.« Back to 2017 American Transplant Congress
